Biomedical Engineering Reference
In-Depth Information
Measured temperature (ºC)
0.1
-0.1
-20
20
40
60
80
100
0
-0.3
-0.5
-0.7
Water (Hindman 1966)
Brain (
ex vivo
canine)
-0.9
-1.1
FIGURE 3.3
Calibration of the proton resonance frequency shift. The measured proton resonance frequency shift versus temperature is plot-
ted for the experiments of Hindman for water along with
ex vivo
normal canine brain heated using a 980-nm cooled laser-applicator at 1.5T with
measurements from a fluoroptic probe and fast chemical shift imaging sequence (Taylor 2011). The temperature sensitivity coefficient is taken from
the slope of the fitted line, which in this case is -0.0103 ± 0.00007 ppm/°C for the canine brain (
R
2
= 0.998) and -0.0103 + 0.00016 ppm/°C for water
(
R
2
= 0.996).
scan echo-planar spectroscopic imaging (LSEPSI) technique on a
mayonnaise and lemon juice phantom also found a similar TSC
when using bulk methylene as an internal reference (McDannold
et al. 2001). More recently, a rapid CSI technique using a multi-
gradient echo showed a similar temperature sensitivity of -0.0088
ppm/°C in a similar fat-water phantom (Taylor et al. 2008). This
is an important finding in that it suggests that if lipid is present in
the tissue, the lipid susceptibility effect corrections are necessary
in order to give more accurate measurements. Basic suppression
of lipid or selective excitation of water for PRF-based temperature
measurements will not suppress the effects from lipid since water
will still experience susceptibility from the lipid. Correcting for
the susceptibility by using lipid as a reference provides higher
accuracy and should be considered when monitoring therapies in
fatty tissues that require high accuracy.
It is also important to note that the PRF sensitivity does not
change when tissues coagulate, which is in contrast to what
is seen in the majority of other parameters (Peters et al. 1998;
Kuroda 2005). This is important with respect to safety aspects as
the ability to measure temperature after damage has occurred is
necessary to assure temperatures do not reach excessive levels,
particularly near high-temperature ablation applicators where
tissue charring can occur.
There is also growing interest in trying to use the PRF, and
particularly CSI, for absolute temperature estimations. Currently,
MRTI methods are used to measure relative temperature changes,
not the actual tissue temperature. Absolute temperature estima-
tion is an established method in NMR experiments. For instance,
in a sample tube, the shift between ethyl (-CH
2
-CH
3
) or methyl
(- CH
3
) protons to the hydroxyl (-OH) protons is commonly used in
the NMR setting. For MR, the goal is to quantify water, lipid, and/
or metabolite peak locations and the relative differences between
them to make absolute temperature measurements (Figure 3.4).
There are studies where N-acetylaspartate and water were used to
measure temperature in the brain with low spatial and temporal
resolution (Cady et al. 1995; Corbett et al. 1995). However, there
are many factors that affect the distribution of the metabolite,
Bulk
methylene
Water
∆f
Te rminal
methylene
Methyl
-2.4
-1.2
0.0
1.2
2.4
Relative PRF (ppm)
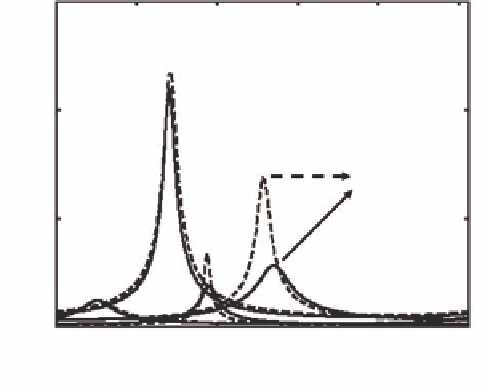
FIGURE 3.4
Lipid-water spectrum. The chemical shift spectrum of
laser irradiated bone marrow
ex vivo
as observed during fast chemi-
cal shift imaging during heating. The spectrum is aliased (i.e., lipid
is shown to the left of water) owing to spectral undersampling by the
sequence. As temperature increases, the water peak shifts from its origi-
nal position (dashed line) to a new position (solid line). The tempera-
ture difference can by calculated from the frequency difference (Δ
f
) and
knowledge of the temperature sensitivity coefficient. Covalently bonded
lipid protons do not shift significantly with heating and thus may serve
as an internal reference to correct for background shifts in the field.