Biomedical Engineering Reference
In-Depth Information
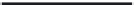
TABLE 17.4
Summary of MagForce NanoTherm Therapy Clinical Trials Completed as of 2011
Start
Ye a r
Tolerable Field
(kA/m)
Median
T90 (°C)
Median
CEM (min)
Phase
Indication
Patients
Adjunct herapy
Implantation Guidance
2003
Phase I
Recurrent Glioblastoma
Multiforme
14
Radiotherapy
StealthStation
®
3.8-13.5
40.5
7.7
2004
Phase I
Recurrent Prostate
Carcinoma
10
—
TRUS, X-fluoroscopy
3-5
40.1
7.8
2004
Phase I
Recurrent Prostate
Carcinoma
8
Brachytherapy
TRUS, X-fluoroscopy
3-5
39.9
5.8
2004
Phase I
Rectal and Cervical
Carcinoma, Sarcoma
Prostate Carcinoma
Cervical Carcinoma
6
8
8
Chemoradiotherapy
Brachytherapy
Chemoradiotherapy
CT
TRUS, X-fluoroscopy
Intraoperative
Pelvic: 3-5
Thoracic: <7.5
NA
NA
2004
Phase I
Hepatocellular
Carcinoma
13
Chemotherapy
Transarterial Infusion
NA
2005
Phase II
Recurrent Glioblastoma
Multiforme
66
Radiotherapy
StealthStation
®
NA
NA
NA
2006
Phase I
Incurable Esophageal
Carcinoma
2
9
—
Chemoradiotherapy
Endoscopic
~3.6
NA
NA
NA = data not yet available
Sources:
Dudeck, O., K. et al.,
Investigative Radiology
41, 6, 2006; Wust, P. U. et al.,
International Journal of Hyperthermia
22, 8, 2006; Johannsen, M. B. et al.,
International Journal of Hyperthermia
, 0, 2006; Steinbach, M. et al., Nanotherapy induced hyperthermia in advanced esophageal cancer: Results of a Phase I
Study, in draft; Maier-Hauff, K. et al.,
Journal of Neuro-Oncology,
2011; Maier-Hauff, K. et al.,
Journal of Neuro-Oncology
81, 1, 2007.
Although, the results have generally been promising, some
side effects were encountered. In many cases, unwanted heat-
ing occurred at the skin or bone interfaces, generally result-
ing in discomfort, but occasionally causing superficial burns.
Other side effects have included tachycardia, headaches, elevated
blood pressure, focal convulsions (Maier-Hauff et al. 2011), and
acute urinary retention (Johannsen, Gneveckow, Taymoorian,
Thiesen et al. 2007). In addition, in current practice, the con-
centrations of iron oxide required to create therapeutic tem-
peratures is much higher than those optimally predicted by
theory, so there is significant opportunity for increasing the
heating efficiency of the nanoparticles used.
maximum intratumoral temperature was 44.6°C and T
90
ranged
from 39.3 to 45.5°C, with a median of 40.5°C. Median calcu-
lated CEM43 was 7.7 minutes. There was no measurable increase
in skin temperature, but body temperature increased by 1.0 to
1.5°C on average.
Implantation and treatment were well tolerated, with no signs
of systemic toxicity. Median patient survival was 14.5 months,
which was promising compared to survival prognoses rang-
ing from 2.7 to 11.5 months. With appropriate consent, histol-
ogy was performed on sections of the treated tissue after death
(van Landeghem et al. 2009). Multifocal deposits were found in
the necrotic regions of the treated tissue. There was significant
uptake by macrophages, and the aggregates were partially sur-
rounded by rings of macrophages. The glioblastoma cells dem-
onstrated uptake to a lesser extent, with only about 5% of cells
containing nanoparticles. Hemorrhage was also found along
the canals of instilled nanoparticles. One patient did not receive
thermal treatment due to health complications after implantation,
and the postmortem histology showed significantly decreased
phagocytotic activity, compared to patients receiving hyperthermia
treatment.
Phase II study has also been completed on 66 patients with
glioblastoma multiforme (Maier-Hauff et al. 2011). The primary
endpoint was survival following diagnosis of first tumor recur-
rence (OS-2), with a secondary endpoint of survival after primary
diagnosis (OS-1). The same methods and procedures were uti-
lized as in phase I study. Patients received six biweekly thermal
treatments with fractionated radiotherapy occurring directly
before or after, with median overall dose of 30 Gy. Median peak
treatment temperature was 51.2°C, with an overall maximum
17.5.2.1 Glioblastoma Multiforme
Phase I and phase II trials have been completed investigating
MFH for treatment of glioblastoma multiforme in combina-
tion with fractionated radiotherapy (Thiesen and Jordan 2009;
Maier-Hauff et al. 2007). The phase I trial included 14 patients
with locally recurrent or nonresectable tumors. Patients received
between 4 and 10 biweekly thermal treatments, depending on
the total weeks of irradiation. Single radiotherapy fractions
of 2 Gy were administered, for complete dosage between 16 to
70 Gy.Nanoparticle injection was preplanned and admin-
istered under stereoscopic guidance with StealthStation
®
(Medtronic, Minneapolis, Minnesota). During treatment, field
strength was increased until the patient experienced subjective
feelings of discomfort, the field was reduced, and the tempera-
tures were maintained for 60 minutes. Field strengths from 3.8 to
13.5 kA/m were well tolerated. Invasive thermometry was used
to monitor intratumoral temperature during treatment. Median