Biomedical Engineering Reference
In-Depth Information
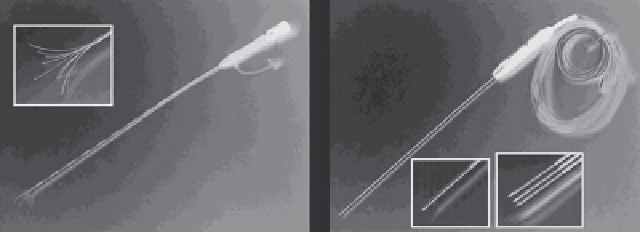
(a)
(b)
FIGURE 9.6
Commercial RF electrodes for tumor ablation. (a) Multi-prong electrode, with magnified electrode tip shown in insert. The prongs
are extended once the catheter is placed in the tumor. (b) Cooled needle electrode, available as single, or three-needle cluster (see magnified
inserts). Active electrode at the tip is 3 cm (single) or 2.5 cm long (cluster), and is internally cooled by circulating water. (Reproduced with permis-
sion from S. Vaezy and V. Zderic, eds.
Image-Guided Therapy Systems
, Artech House, Inc., Norwood, MA, 2009. © 2009 by Artech House, Inc.)
alone (Jemal 2007), and most patients are not surgical candi-
dates; recent studies suggest that patients with inoperable lung
cancer may benefit from RF ablation (Simon 2007, Gillams
2008). A tumor ablation procedure can be performed minimally
invasively through a small incision in the skin (by an interven-
tional radiologist), or during laparoscopy or open surgery (by a
surgeon). During the procedure, the patient is typically under
light general anesthesia or conscious sedation and can leave the
hospital the same, or the next, day.
The treatment goal is to thermally ablate tissue in a zone that
encompasses the under imaging visible tumor as well as a ~1 cm
margin of normal tissue to ensure destruction of any cancer
microsatellites that may surround the tumor (Sasaki 2005). For
tumors larger than 3 cm, multiple overlapping ablations created
either sequentially (Chen 2004) or simultaneously with multiple
electrodes (Laeseke 2007) are typically required.
Limitations of current RF tumor ablation procedures include:
e.g., for different types of tachycardia (fast heart rhythm above
150 bpm) and atrial fibrillation (i.e., quivering of the atria)
(Huang 2006, Wilber 2007). The spatiotemporal activation
pattern of the heart is determined by a specialized conduction
system, and abnormalities in electrical conduction in the heart
can result in arrhythmia. The goal of cardiac RF ablation is to
destroy a small region of heart tissue to normalize electrical
activation in the heart (e.g., by destroying additional conduc-
tion pathways not present in a normal heart).
Cardiac ablation is performed in a specifically equipped
interventional laboratory by an electrophysiologist. A cath-
eter is inserted into a vessel (typically in the groin or neck) and
steered into the heart (Figure 9.7). The procedure is guided by
x-ray imaging. In addition, electrical measurements of local
cardiac activity (similar to ECG) are performed via recording
electrodes located on the RF catheter (Figure 9.8), as well as
by additional specialized recording catheters placed at various
locations in the heart. Through these local electrical activity
measurements, temporal activation patterns of the heart can be
determined to diagnose the cause of the arrhythmia and site
that needs to be ablated. Subsequently, the RF catheter is steered
to the target site and RF current is applied to the heart tissue for
~45-120 s, creating an ablation zone of ~5-10 mm in diameter
(Figure 9.9).
For most commercially available catheters, the applied RF
power is adjusted depending on temperature measured by a sen-
sor located within the electrode tip (temperature control). Note,
however, that electrode tip temperature is lower than the maxi-
mum temperature within the tissue (see Figure 9.9). This is of
importance because one of the undesired effects that can occur
is tissue perforation (often called “popping” due to the sound
associated with this event), which is due to tissue vaporization
above 100°C. Intracardiac blood flow (i.e., blood velocity at
the electrode) considerably affects tissue heating and resulting
size of the ablation zone (Figure 9.10). Usually, larger ablation
zones are possible at locations with high blood flow (Cao 2001,
Tungjitkusolmun 2001, Petersen 1999). To create ablation zones
of varying dimensions, catheters of different lengths and diam-
eters are commercially available. Some newer catheter designs
1. limited performance close to large vasculature, that may
result in tumor recurrence due to inadequate temperatures;
2. inadequate intra-procedural imaging feedback on abla-
tion zone growth;
3. the size of the ablation zone of a single ablation is often
not adequate to treat large tumors (>3 cm diameter),
resulting in prolonged procedural times and higher
recurrence rates.
9.3.1.1 radiofrequency Electrodes for tumor ablation
There are a number of different electrodes commercially avail-
able. Some electrodes have multiple tines that are extended
after the electrode is inserted into the tissue (Figure 9.6a), while
another kind uses needle electrodes that are internally cooled
(Figure 9.6b). Most of the electrode shaft is insulated such that
tissue heating is only produced at the most distal electrode por-
tion (see inlets in Figure 9.6).
9.3.2 Cardiac arrhythmia treatment
RF ablation (cardiac RF catheter ablation) is frequently used for
treatment of cardiac arrhythmia (i.e., irregular heart beats),