Biomedical Engineering Reference
In-Depth Information
A general conclusion of the fracture healing and
stress shielding research is that desirable micro-
motion to enhance bone healing and maintain healthy
bone porosity is limited with the use of any rigid
metallic fixation. As discussed previously, from the
standpoint of fracture healing, it can be beneficial to
utilize semirigid internal fixation, allowing some
motion in specific directions. However, when
considering stress shielding, it seems more desirable
to fixate bone fractures with a material that is close in
mechanical stiffness to that of healthy bone.
Although exact requirements for rigidity are still
being sorted out, attempts have been made to estab-
lish some guidelines. For example, in the load-
bearing lower extremities, it has been recommended
to provide fixation of 43
e
53% that of stainless steel,
while in the forearm this percentage is approximately
30%
[10]
. What is certain is that a better under-
standing of how fractures heal and how bone main-
tains itself continues to support the concepts of
semirigid and biologic fixation. As we will see,
PEEK is an exciting option for application within
these two concepts.
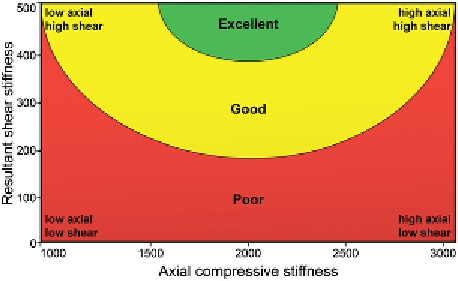
Figure 15.2
A plot of resultant shear stiffness vs. axial
compressive stiffness adapted from Epari et al.
[6]
. The
contours indicate areas of similar healing outcome and
describe the ideal healing environment as having
maximal shear stiffness and moderate axial compres-
sive stiffness.
plates for titanium, while others yet have decreased
the profile and bending stiffness of the implant
hardware. These have all been promising develop-
ments on the biologic fixation front, as the older
concepts of maximum mechanical stability had been
the primary design goal working against minimally
intrusive fixation. As we will see in the next section,
problems with overly stiff permanent hardware can
extend well past the initial healing period.
15.2.3 Semirigid Fracture
Fixation Plates
“Semirigid” carbon-fiber-reinforced (CFR) poly-
mer fracture fixation plates were developed starting
in the 1980s as an alternative to comparatively
“rigid” stainless steel bone plates
[11
e
16]
.As
a historical note, an investigation of CFR polymer
fracture fixation plates was reported by Bradley et al.
[16]
in the first published issue of Biomaterials.A
commercial epoxy prepreg resin was chosen as the
polymer matrix for the plates, and these implants
exhibited 1/3 of the bending stiffness and 10%
greater flexural strength than steel plates. The
biocompatibility of CFR epoxy plates was confirmed
to be comparable with stainless steel plates by testing
biopsy samples from tissue obtained when the
devices were surgically removed following fracture
healing
[17]
. However, an important disadvantage of
a thermosetting polymer, such as epoxy, is its
inability to be contoured to the bone fragments of
a fracture, rendering it less clinically useful than
metallic or polymeric plates that have this capability.
High-performance thermoplastic materials,
including nylon 6-10, polybutylene terephthalate
(PBT), polysulfone (PS), and PEEK, were also
extensively studied as candidates for fracture fixation
15.2.2 Stress Shielding After
Fracture Healing
After a successful bone union with an internal
fixation treatment, the stiffness mismatch between
the fixation device and the bone can continue to cause
the implant to transmit the majority of stress. The
underlying bone will continue to adapt to its altered
mechanical environment. Wolff's Law dictates that
the density of bone is dependent on its stress condi-
tion
[7]
. If the applied stress environment of a load-
bearing bone region is decreased below its normal
physiological levels, the bone density of that region
can decrease leading to a reduction in strength, the
degree of which is directly related to the stiffness of
the implant material
[8,9]
. The effects of stress
shielding on a healed bone begin with the resorption
of bone on the endosteal cortex, followed by
a widening of the medullary canal and a thinning of
the cortices
[9]
. Clinically, stress shielding can
decrease local bone mineral mass and may lead to
either failure of the fixation or refracture of the bone
after plate removal
[3,8,10]
.