Biomedical Engineering Reference
In-Depth Information
stimuli, sex, age, metabolic status, and lifestyle factors
[3]
. The treatment goal is to create the best biologic
environment to facilitate healing. Depending on the
mechanical environment, a fracture can either undergo
primary or secondary healing. Primary healing
involves a direct attempt of the cortex to reestablish
itself without callus formation. Secondary fracture
healing includes an intermediate callus stage. Primary
healing is often slower and certainly rarer, as it is
considerably more difficult to achieve in most load-
bearing bones. Resultantly, an uneventful secondary
healing process is often the goal of treatment.
For secondary fracture healing, there are three
stages: (1) inflammation, (2) reparation, and (3)
remodeling.
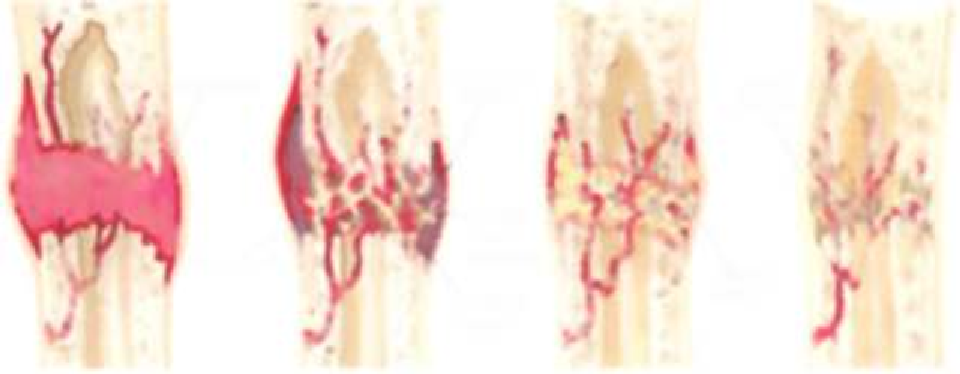
Figure 15.1
is a graphic depiction of the
healing bone. After a fracture, the supply of blood
and oxygen to the region is greatly increased. The
inflammation stage starts immediately with a hema-
toma or blood clot forming at the fracture site. The
hematoma will seal off the fractured edges, causing
the death and lysis of local osteocytes. The hema-
toma provides a small amount of mechanical stability
and contains precursor mesenchymal stem cells that
will eventually generate into osteoblasts, chon-
drocytes, fibrocartilage, or fibrous tissue. In the first 2
to 3 days, a fibrous granulation tissue forms. At the
same time, inflammatory clean-up cells, osteoclasts
and macrophages, are dissolving and removing
damaged and necrotic tissue. Resorption widens the
gap and lowers the strain to levels that can be toler-
ated for
Resorption seems to be strain dependent, as areas of
elevated tissue strain have been directly correlated to
the spatial distribution of bone resorption in sheep
[2]
. At about 2 weeks, the reparation phase begins. At
this time, the proteins produced by the repair cells
begin forming a soft (fibrocartilaginous) callus of
osteoid and cartilage. Calluses are fibroblasts and
chondroblasts that form at the area of bone fracture.
The cells eventually dissipate and lie within the
extracellular matrix that becomes bone. The callus
will momentarily bridge and stabilize the fracture
gap. New matrix formation can occur as intra-
membranous or endochondral ossification as the
callus hardens into a combination of woven and
lamellar bone as bone spicules fuse into trabeculae
over the next 6 to 12 weeks. Finally, the remodeling
phase completes as the trabecular bone remodels into
compact bone according to a balance of formation
and resorption from osteoblast and osteoclast
activity. A clinical union of bone will occur as
secondary lamellar bone formation at 12 to 16 weeks.
At this time, the fracture site will have normal bone
stiffness and strength.
15.2.1 Mechanical Stability in
Fracture Healing
Although the process through which bone heals is
well understood, the understanding of requirements
for safe and timely fracture healing has continuously
morphed over the years, and still remains somewhat
the beginning of
tissue differentiation.
Figure 15.1
Illustration of fracture healing stages including, from left to right, the formation of a hematoma at the frac-
ture site, callus formation and the hardening of callus into woven and lamellar bone spicules, consolidation of bone
spicules into a matrix of trabeculae bone, and remodeling of the trabeculae bone into compact bone and a clinical
union.