Biomedical Engineering Reference
In-Depth Information
14.3 Setbacks with Early
PolymereMetal Composite Hip
Stems
The measured adoption of PEEK biomaterials in
hip stems has been tempered by previous experience
with the historical failures of isoelastic and Proplast-
coated hip prostheses in the 1970s and 1980s, and,
most recently, isoelastic polysulfone composite stems
in the 1990s. The concept of a cementless “isoelastic”
hip stem was reportedly conceived in 1967 by Robert
Mathys as an alternative to the cemented metallic hip
implant design developed by Sir John Charnley
[4,5]
.
The isoelastic hip stem was intended to replicate the
stiffness to the femur, to reduce stress shielding and
improve implant fixation. The first isoelastic hip
design, clinically implanted starting in 1973, was
a composite prosthesis consisting of a polyacetal
copolymer with a tapered metallic core (Factory for
Surgical Instrumentation, Bettlach, Switzerland). This
device was inserted without cement, and used a prox-
imal lag screw for fixation. Loosening of this pros-
thesis, attributed to poor clinical technique and
excessive proximal micromotion, also led to a second,
and ultimately a third generation of the RMI
Cementless Hip Prosthesis
[4,5]
. These subsequent
generations differed in geometric design, but retained
the same polyacetal copolymer fixation interface.
Despite encouraging short-term clinical results
[4,5]
,
longer investigation, with an average follow-up of 42
months, revealed unacceptably high rates of mechan-
ical loosening for the third-generation RMI prosthesis
[9]
. By 1988, Jakimet al.
[9]
noted that “the concept of
isoelasticity that has attracted many surgeons has
failed to fulfill original clinical expectations.”
Investigation of the retrieved periprosthetic tissues
from revision surgery patients demonstrated the
presence of polyacetal, polyethylene, and metal
particles. Extremely large foreign-body giant cells
were noted to be associated with polyacetal particles
[10]
. A later study confirmed that the adverse tissue
response was more intense for the polyacetal stems
than for CoCr stems
[11]
. The authors concluded that
increased stresses and micromotion at the proximal
calcar and the resulting generation of wear debris
(polyacetal and barium sulfate radiopacifier)
contributed to the poor long-term clinical perfor-
mance of the RMI stem. It is notable that the suit-
ability of polyacetal (Delrin) has been questioned for
orthopedic applications
[12,13]
.
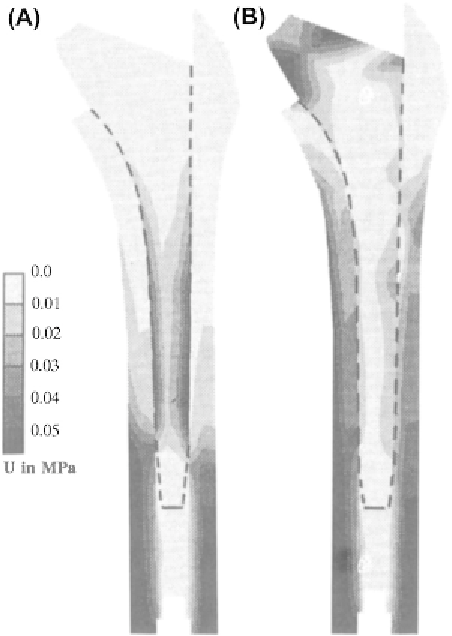
Figure 14.2
(A) Strain energy distribution in stem and
bone with CoCrMo prosthesis (a) and “isoelastic”
prosthesis (b). The average strain energy density from
three loading cases is shown. (B) Normal interface
stresses before and after simulated bone remodeling
for CoCrMo and “isoelastic” uncemented stems.
Images reproduced from Ph.D. thesis with permission
from Harrie Weinans, Ph.D.