Biomedical Engineering Reference
In-Depth Information
Chapter 13
Applications of Polyaryletheretherketone
in Spinal Implants: Fusion and Motion
Preservation
Steven M. Kurtz Ph.D.
13.1 Introduction
spine while the bone fused across the treated
level
[3]
.
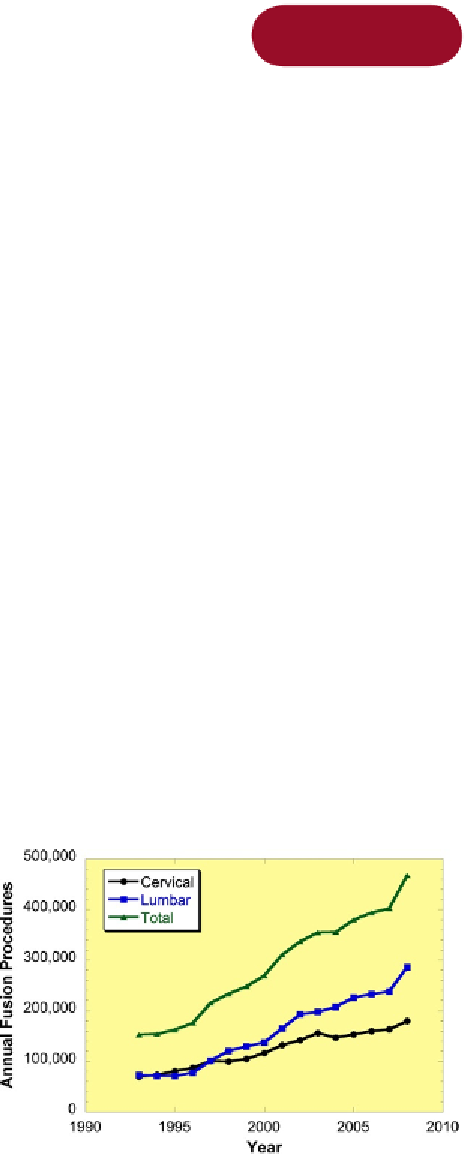
Since the 1990s, the incidence of spinal fusion has
grown substantially in the United States
[4]
, reflect-
ing both an increased prevalence of the degenerative
disc disease and growing acceptance of the procedure
(
Fig. 13.1
). In 2008, an estimated 286,000 thor-
acolumbar fusions and 180,000 cervical fusions were
performed in the United States based on the data
from the Nationwide Inpatient Sample (NIS), and
that the number is projected to increase to millions of
procedures a year within the next two decades
[5]
.
Polyaryletheretherketone (PEEK) interbody cages
represent a considerable commercial, as well as
clinical, success. The US market for interbody fusion
products has increased from 0.6 billion US$ in 2004
The orthopedic and biomaterials literature of the
1990s reflects an early academic curiosity in implant
applications of polyaryletherketone (PAEK) bioma-
terials
[1,2]
. However, widespread commercial
applications for PAEK biomaterials in the human
body were first realized with cage implants intended
to promote intervertebral body (interbody) fusion of
the lumbar spine. Success of PAEK with interbody
implants would later inspire applications in a broad
variety of spinal implant applications, including
posterior fusion, dynamic stabilization, and disc
arthroplasty.
Fusion is now considered a standard of care for
intractable low back pain arising from degenerative
disc disease and/or spinal instability. In the cervical
spine, anterior decompression and fusion is the
standard treatment for degenerative disc disease,
myelopathy, and radiculopathy. Whether in the
lumbar or cervical spine, fusion consists of first
immobilizing the painful spine segments by encour-
aging bone growth across the immobilized level.
Spine fusion was first performed without instru-
mentation using bone grafts, often obtained from the
patient's own body, such as iliac crest. Harvesting
bone from the patient was undesirable, because it is
a second procedure and has associations with
complications, including donor site pain. Also, the
operated level was unstable until fusion occurred,
and required local immobilization. Posterior instru-
mented fusion, using rods, plates, and screws, was
developed to provide immediate rigid stability to the
Figure 13.1
Incidence of spinal fusions in the United
States based on NIS data from 1993 to 2008. Source:
http://hcupnet.ahrq.gov
.