Biomedical Engineering Reference
In-Depth Information
17.6.1 B
IOINERT
M
ATERIALS
IN
B
LOOD
-C
ONTACTING
D
EVICES
For a long period of time, the most accepted strategy to produce a successful blood-contacting
device was to make use of materials to which no proteins would adsorb or no cells would interact
with. This bioinert principle was based on the idea that when blood would not interact at all with the
material, no adverse response could take place and therefore no complications of the device would
occur.
58,59
It soon turned out that the favorite materials of the industry like poly(tetrafl uoroethylene)
(PTFE; Tefl on) or poly(ethyleneterephthalate) (PET) were not as inert as they were thought to be
(Figure 17.10). The manufacturers advertising for Tefl on-coated frying pans claim that no substance
would stick to it. This may be true at high temperatures, but when applied in a patient, proteins and
cells will readily interact with Tefl on surfaces. This does not mean that no successful implants con-
sisting of PTFE or PET have been produced. Best known among them are the large diameter blood
vessels (
5 mm inner diameter) made of PET or PTFE.
60,61
Especially prostheses that are intended
to replace the aorta upon rupture, or in case of severe aortic aneurysms, have been very successful,
saving many lives. Also the carotid or femoral arteries are frequently replaced by PTFE prosthe-
sis.
62
The success rates depend on the health of the patient and the fl ow regime of the intended site
of implantation. The higher the blood fl ows, the more chance of success since possible activators of
coagulation are rapidly diluted under high blood fl ow.
Intravenous catheters are often made of polyvinylchloride (PVC) (Figure 17.10) and are vital for
the application of drugs, fl uids or nutrients to patients. The vast majority of these catheters remain
in the vessel for only a couple of days, but some are inserted for several months into the large
veins in the chest. The most common problems of these catheters are infection and coagulation.
Therefore, these tubes are frequently fl ushed with the anticoagulant heparin. Infection can be
treated with antibiotics, but in some severe cases the catheter has to be removed. So one can see that
it is a challenge to design materials, which prevent coagulation and, at the same time, adhesion of
bacteria. It has been shown that though inert materials perform reasonably well, eventually proteins
and bacteria will adsorb and cause failure of the device.
Also polyurethanes are used or studied for blood-contact devices.
63
The advantage is that poly-
urethanes are a very versatile group of polymers. These materials are so-called block copolymers
that contain soft and hard blocks. The easy chemical synthesis facilitates the design of materials
with a variety of surface characteristics and mechanical properties. The disadvantage is that some
of polyurethanes are degraded inside the body and that the degradation products often cause a
severe infl ammatory response.
64
The use of polyurethanes in blood contact devices is still under
investigation and some positive studies have been reported for vascular prostheses.
63
A new area of interest is the application of nanostructured surfaces of these materials. It has
been shown that submicromolar or nanostructures can modulate the adhesion and viability of cells
and bacteria. It remains to be determined how these surface topographies can be applied to manipu-
late the interaction of blood and cells with synthetic surfaces.
>
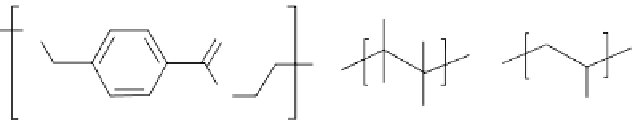
PVC
PET
PTFE
F
F
O
O
n
n
O
F
O
Cl
n
F
FIGURE 17.10
Structure of poly(ethyleneterephthalate) (PET), Tefl on or poly(tetrafl uoroethylene) (PTFE),
and polyvinylchloride (PVC).