Biomedical Engineering Reference
In-Depth Information
Blood will quickly coagulate to prevent excessive blood loss. Formation of blood clots will also
occur on the surface of the implant, changing its surface characteristics. Apart from wound healing
and tissue regeneration, blood plays a vital role in the immune response toward synthetic materials
and devices, delivering cells of the immune system to the site of implantation.
For devices that are intended to function in direct contact with blood, an optimal interaction
with blood (blood compatibility) is essential. Blood coagulation, infl ammation, or uncontrolled tis-
sue formation are the most common problems encountered with blood-contacting devices, seriously
threatening the function of the device and consequently the health of the patient.
Biomedical engineering has come up with a number of strategies to minimize complications of the
blood, like infl ammation and coagulation. Thus it is important to understand the interaction between
blood and the surface of implants to be able to design biomaterials that display an acceptable interac-
tion with blood. In this chapter the interaction of blood with synthetic surfaces will be described. The
most commonly used strategies that aim to optimize blood compatibility of synthetic surfaces are
discussed as well as the methods to determine effi ciency of these blood compatibility strategies.
17.2 BLOOD
Blood is a complex mixture of plasma (containing a large number of proteins, lipids, ions, etc.) and
cells (erythrocytes, leukocytes, and platelets).
1
-
3
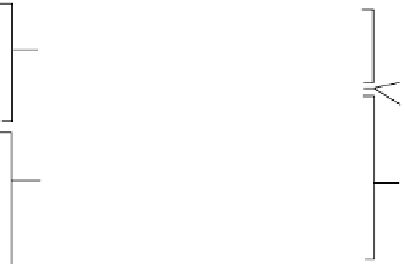
Blood can be easily divided into its major components
by centrifugation, since cells have a somewhat higher density than platelets and plasma (Figure 17.1).
The use of full blood is preferred for studying the performance of blood-contacting devices,
prior to implantation. For simplicity and for practical reasons often platelet-rich plasma (PRP)
and platelet-poor plasma (PPP) are used. Microscopy is much easier using the translucent PRP or
PPP. Also the use of spectroscopic techniques is almost impossible using whole blood, because the
erythrocytes scatter light.
The different cells in the blood are formed in the bone marrow by a process called hemopoiesis.
3,4
Pluripotent hemopoietic stem cells (PHSC) have the ability to differentiate into all cell types present
in the blood.
3,4
1800
g
/10 min
180
g
/15 min
Platelet-rich plasma
(PRP)
Platelets
Platelet-poor plasma
(PPP)
Leukocytes
Platelets
Leukocytes
Erythrocytes
Erythrocytes
FIGURE 17.1
Blood can be divided into different parts. Centrifugation at 1800
g
will result in platelet-poor
plasma (PPP) resting on top of the erythrocytes that occupy approximately 40-50% of the total blood volume.
Platelet-free plasma (PFP) can be obtained by further high-speed centrifugation of the PPP. Leukocytes and
platelets form the so-called buffycoat, the boundary layer between plasma and erythrocytes. Centrifugation at
180
g
will result in approximately 30-35% of volume PRP, containing 300
-
500
×
10
6
platelets/mL.