Biomedical Engineering Reference
In-Depth Information
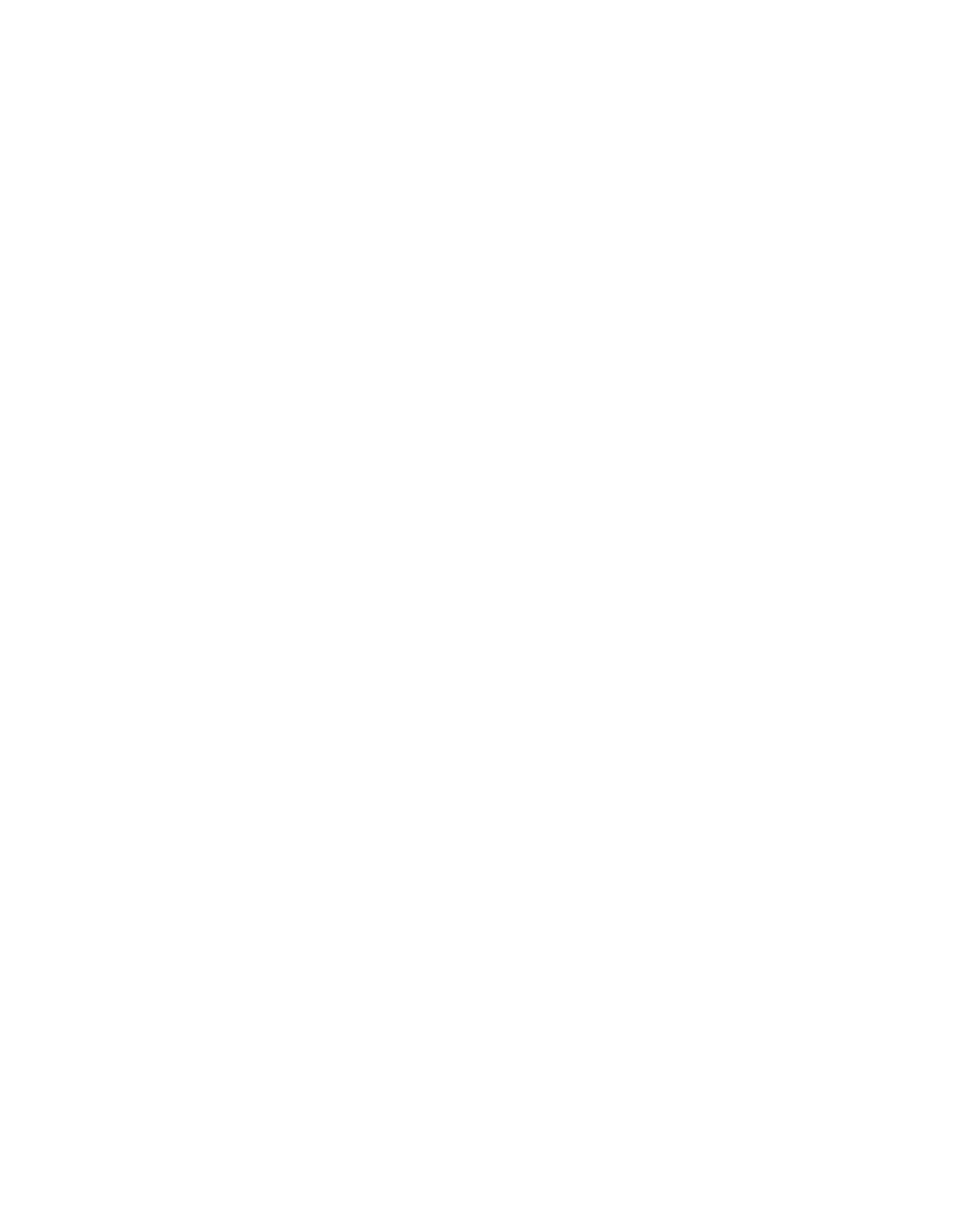
TABLE 1.3
Comparison of Mechanical Properties of Calcium Phosphates and Human Bone
Compressive
Strength
(MPa)
Fracture
Toughness
(MPa
√
__
Tensile Strength
(MPa)
Elastic Modulus
(GPa)
Ceramics
m )
References
Calcium phosphates
20-900
30-200
30-103
<
1.0
39,42
Hydroxyapatite
>
400
∼
40
∼
100
∼
1.0
39,42
Cortical bone
130-180
50-151
12-18
6-8
28,43-46
higher stiffness, higher compressive and tensile strength, and greater fracture toughness [39,40].
It has been reported that the fl exural strength and fracture toughness of dense hydroxyapatite are
much lower in a dry condition than in a wet condition [41]. The mechanical properties of hydroxy-
apatite and related calcium phosphates, as well as those of bone, are given in Table 1.3.
In brief, hydroxyapatite and related calcium phosphates exhibit excellent biocompatibility and
osteoconductivity. However, these materials are poorly degradable in case of crystalline structures,
and their amorphous counterparts are mechanically too fragile to be used for fabrication of highly
porous tissue-engineering scaffolds.
1.3.2 B
IOCERAMICS
: B
IOACTIVE
S
ILICATE
G
LASSES
1.3.2.1 Biocompatibility
As early as in 1969, Hench and colleagues discovered that certain silicate glass compositions had
excellent biocompatibility as well as the ability of bone bonding [23-25]. Through interfacial and
cell-mediated reactions, bioactive glass develops a calcium-defi cient, carbonated calcium phosphate
surface layer that allows it to chemically bond to the host bone. This bone-bonding behavior is
referred to as “bioactivity” and has been associated with the formation of a carbonated hydroxy-
apatite layer on the glass surface when implanted or when in contact with biological fl uids [47-50].
Bioactivity is not an exclusive property of bioactive silicate glasses. Hydroxyapatite and related
calcium phosphates also show an excellent bone-bonding ability, as discussed above. The capability
of a material to form a biological interface with the surrounding tissue is critical in avoiding scaf-
fold loosening
in vivo
.
Bioactive glasses have also been found to support enzyme activity [51-54], vascularization
[55,56], as well as foster osteoblast adhesion, growth, and differentiation. Bioactive glasses were
also shown to induce the differentiation of mesenchymal cells into osteoblasts [57-59] and to pro-
vide osteoconductivity [60].
A signifi cant fi nding for the development of bone engineering is that the dissolution products
from bioactive glasses exert a genetic control over osteoblast cycle and rapid expression of genes
that regulate osteogenesis and the production of growth factors [61,62]. Silicon has been found to
play a key role in the bone mineralization and gene activation, which has led to the substitution
of silicon for calcium into synthetic hydroxyapatite. Investigations
in vivo
have shown that bone
ingrowth into silicon-substituted hydroxyapatite granules was remarkably greater than that into
pure hydroxyapatite [62,63].
The above-mentioned advantages make 45S5 Bioglass a very successful material in clinical
applications, for example, for the treatment of periodontal disease (PerioGlas) and as a bone-fi ller
material (NovaBone) [63,64]. Bioglass implants have also been used to replace damaged middle
ear bones, restoring auditory capabilities of patients [64]. Recently bioactive glasses have gained
attention as promising scaffold materials for bone tissue engineering [64-69]. Similar to calcium
phosphates, the application of this material, particularly in tissue engineering, has encountered a