Biomedical Engineering Reference
In-Depth Information
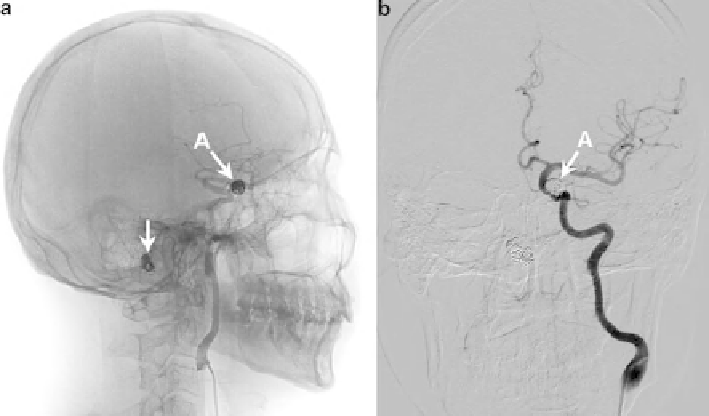
Fig. 1 Endovascular coiling of cerebral aneurysms: (a) the location of two coiled aneurysms
(indicated by
arrows
); (b) DSA examination reveals occlusion of the aneurysm from the parent
artery
(Fig.
1
b). The aim is to prevent blood from flowing into the intra-aneurysmal space,
thus to reduce aneurysm rupture risks.
In preoperative plannings, interventionists often construct the blood flow
“image” from mind to judge the potential complications [
2
]. With the advance of
medical imaging technologies and computing capacity, it is now feasible to simu-
late blood flow in blood vessels in a patient specific manner (e.g., see [
3
,
4
]).
Furthermore, a computer model can simulate some clinical scenarios which are
otherwise expensive to experiment in vitro (e.g., mechanical analysis of different
stent strut designs [
5
]), or too risky to perform in actual clinical procedures
(e.g., balloon occlusion tests in vivo [
6
]).
The problem with a computational tool, however, is that it must be highly
efficient to fit in a clinically relevant timeframe. Also, the computer model should
reflect a patient's actual vascular anatomy, i.e, be patient-specific. These two
desired features are often contradictory in terms of implementation: a higher fidelity
to vascular geometry will certainly demand more computing resources. For
instance, it can take days or even weeks to compute the complex 3D flow patterns
in arterial trees on a high-end computer system [
3
]. Therefore, a tradeoff must be
made between the computational cost and vascular model accuracy.
Some efficient numerical methods for solving flow in large vasculatures have
been proposed, e.g., the one-dimensional (1D) models in [
7
] and [
8
]. These 1D
models reduce the computational time from hours or days to minutes. The
objective of this paper is to check the feasibility of using a 1D model for
haemodynamic simulations in endovascular procedures. Firstly, we brief the