Biomedical Engineering Reference
In-Depth Information
at the end of 30 min of iontophoresis (0.4 mA/cm
2
). LHRH transport in a pulsatile
manner was achieved by repeated processes of one pulse, immediately followed by
30 min iontophoresis. Skin toxicity of electroporation together with iontophore-
sis evaluated. Pulses of 0, 250, 500, and 1000V were applied, followed by constant
current anodal iontophoresis of 0, 0.2, and 2.0 mA/cm
2
for 30 min or 10 mA/cm
2
for
10 min. At the gross microscopic level, immediately after or 4 h after treatment, ery-
thema increased with increasing pulse voltage. Erythema, edema, and petechiae all
increase significantly with increased current in the absence of a pulse. The application
of an electroporation pulse did not increase the iontophoretic-induced irritation with
any current tested. All skin changes tended to decrease within 4 h after the treatments.
Nevertheless, at times lowered combined effects in contrast to the effects achieved
with each individual treatment were also reported. Denet et al. reported lowered
transdermal delivery of the hydrophobic drug timolol with iontophoresis and elec-
troporation combination than with iontophoresis alone
[80]
. The decreased transport
was explained as being due to an accumulation of positively charged timolol in the
SC, which was amplified by electroporation, and a resulting decrease of electroos-
motic flux during iontophoresis
[44,80]
. The practical application of combining
electroporation with iontophoresis is still in its initial trial stage, similar to the com-
mercial development of electroporation devices for transdermal delivery of drugs.
Iontophoretic studies have resulted in a few marketed medical device products, some
containing drugs, that are close to FDA approval.
12.1.4.1.2 Skin Microporation
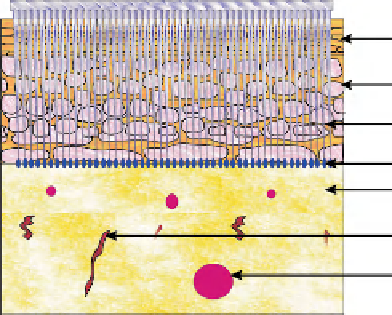
Skin microporation involves the creation of micron-sized micropores or microchan-
nels in the skin that allow the transport of macromolecules and soluble drugs, as
shown in
Fig. 12.6
. Technologies that create these microchannels in the skin include
mechanical microneedles
[81,82]
, thermal or radiofrequency ablation, and laser abla-
tion. The approach looks very promising and is likely to revolutionize transdermal
drug delivery of proteins and peptides.
Microneedle approaches are designed to circumvent the primary skin barrier
without intruding on the underlying pain receptors and blood vessels. Microneedles
Figure 12.6
Schematic
representation of delivery
of a drug through
microneedle-punctured
skin.
Stratum
corneum
Epidermis
Microneedles
Drug
Dermis
Pain receptor
Blood vessel
Search WWH ::

Custom Search