Biomedical Engineering Reference
In-Depth Information
(
A
)
(
B
)
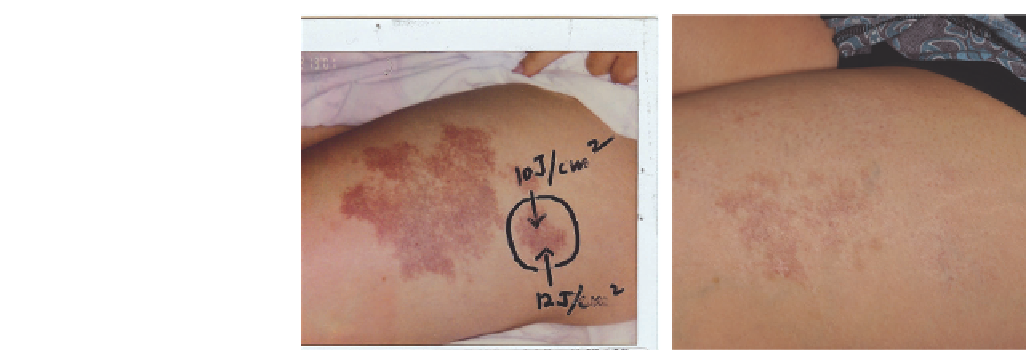
Figure 2.22
Port-wine stain (
A
) before and (
B
) after 25 treatments with potassium titanyl phosphate and pulsed dye laser.
spot overlap, or post-treatment trauma to the site. Almost all
reported cases have resolved spontaneously within 1 year (77).
In terms of potential for laser treatments to disrupt local vas-
cular fl ow and potentially cause glaucoma, initial evidence
suggests that PDL treatments to periocular PWSs do not dem-
onstrate clinically relevant effects on intraocular pressure (110).
Similarly, the theoretical risk of hemoglobinemia that could
result from photothermolysis does not appear to be clinically
relevant. In this scenario, photothermolysis of blood vessels
does result in the release of free HgB into the circulation with
the resulting hemoglobinemia leading to renal impairment in a
young patient. Fortunately, a study of 15 patients under age fi ve
years treated with the PDL-tested serum haptoglobin and urine
hemosiderin postoperatively found that even though patients
had a treatment region more than 3% of total body surface area
and received 5-mm-diameter pulses more than 1500 in some
cases, there was no evidence of urine HgB and serum hapto-
globin levels were normal (111).
“Before” and “after” photos may be particularly useful tools for
demonstrating effi cacy and assuaging fears. If possible, a test area
using a local anesthetic cream and about four to eight laser pulses
(at the lower end of the energy range) may be performed prior to
a full treatment session; this permits families to witness the entire
treatment process and allows the laser surgeon to gauge the skin's
response to laser treatment (109). Caregivers should always be
informed of specifi c aftercare instructions, including follow-up
clinic appointments and additional treatment sessions.
Generally, the smaller, more superfi cial vessels are targeted
with GY light fi rst. Deeper, larger caliber vessels may require
longer pulse durations or longer wavelengths. Purpura (with
GY light sources) is the clinical endpoint of successful laser
treatment for most PWSs (77). However, studies have shown
that purpura-free clearing of PWS is possible with PDL, KTP,
and IPL devices. In all instances, graying of tissue is an indica-
tion of possible overtreatment.
It is not uncommon for an uneven response to PDL to be
seen. Responses may vary according to the gross anatomic
area, the local dermal blood fraction, and the microscopic
anatomy of the lesion. Factors lending themselves to a more
favorable response to treatment include younger age; lighter
pink-red color (in contrast to deep purple); and certain ana-
tomical sites, with lateral facial, periorbital, forehead, chest,
neck, and proximal aspect of arm lesions generally responding
better than PWSs located on the center of the cheeks or on the
more distal extremities (112).
Successful treatment also seems to correlate with timing,
number, and frequency of laser treatment sessions. The fi rst pub-
lished reports of PDL for PWS noted complete clearing of pink-
to-red macular PWS in 35 children younger than 14 years (mean
age 7 years 2 months) with an average of 6.5 treatments (113).
Subsequent clinical studies demonstrated notable effi cacy and
defi ned more reasonable expectations. Reyes and Geronemus
(77) successfully treated 73 patients between age three months
and 14 years. The overall average lightening after one treatment
was 53%, and the percentage of lightening increased with subse-
quent treatments. More than 75% lightening was achieved with
an average of 2.5 treatments in 33 patients.
Morelli and Weston advocate beginning treatment as early
as 7-14 days of age so that three treatments can be done before
the infant reaches six months of age. They noted a 50% resolu-
tion with this protocol by the third treatment. In their popula-
tion of 132 patients, complete clearance was obtained in 25%
of PWSs when treatment was begun before 18 months of age
(average 7.8 treatment sessions) versus 7-10% having total
clearance when treatment was begun between ages 11/2 and
18 years (average 7.0 treatment sessions). A follow-up evalua-
tion of this patient population confi rmed the authors' initial
observations with 83 children: 32% of children who began
treatment before 1 year of age had complete clearing of their
PWS compared with 18% of children treated after 1 year of
age. In this later study, 32% of patients with PWS less than
20 cm
2
in size completely cleared compared with an 8% com-
plete clearance rate in patients with larger PWS (114-116).
Our studies on the treatment of 43 children between ages
2 weeks and 14 years with 49 lesions of capillary malformation
confi rm these results (117). Lesions treated in children under
age 4 years had greater overall improvement with less
treatment sessions compared with those in children over age
4½ years (Table 2.2). In general, improvement and clearance
were gradual and required 5-10 treatments. However, very
superfi cial lesions cleared more quickly, with four lesions
reaching a level of 95% clearing in one or two treatments.
An additional study of 12 children 6-30 weeks of age con-
fi rmed that treatment of infants only a few weeks old can be