Biomedical Engineering Reference
In-Depth Information
or guardian, and informed consent should be obtained. Fami-
lies should be alerted to the possibility of unpleasant dreams
and emergence phenomena for the patient. Such occurrences
should be reported to modify future anesthesia (45-50).
Routine laboratory tests are usually not required. Patients
should be fasting overnight prior to the administration of the
anesthetic, with the exception of clear liquids, which are
allowed 2 hours before the procedure. This regimen can prob-
ably be liberalized further based on certain studies (51). In
patients with acute, resolving, or recent respiratory infections,
the procedure should be postponed until symptoms, especially
nasal secretions and cough, resolve (52).
Premedication
Typically, no premedication is given for the first treatment.
Subsequently, families are given the option of administering
oral diazepam (Valium, 0.1-0.2 mg/kg) preoperatively.
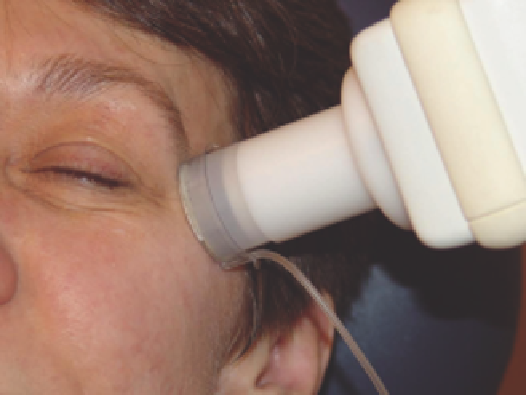
Figure 16.4
Iontophoresis.
Source
: Courtesy of Jaggi Rao, MD.
A complete discussion regarding these requirements is beyond
the scope of this chapter.
Induction/Maintenance/Emergence
The treatment room is prepared as follows. Oxygen E cylinder
is checked and linked to a resuscitation bag. Suction equipment
is assembled and kept ready with both a Yankauer suction and
a soft suction tip. An IV solution of lactated Ringer's solution
with or without 5% glucose with microdrip system is prepared.
Endotracheal tube (ET) and laryngoscope are kept ready. Med-
ications are prepared, including ketamine, midazolam, fentanyl
citrate hydrochloride, glycopyrrolate, atropine, succinylcholine
chloride, droperidol, epinephrine, lidocaine, diphenhydramine
hydrochloride, and others, as needed. Monitors include precor-
dial stethoscope, temperature monitor, Criticare #506 [con-
tains noninvasive blood pressure measurement, pulse oximetry,
electrocardiography (ECG)], and backup manual blood pres-
sure cuff with sphygmomanometer. Ohmeda 9000 continuous/
bolus infusion pump is kept ready with diluted ketamine
solution, usually with milligrams of ketamine three to six
times patient weight in kilograms in a final volume of 20 mL
(Fig. 16.5).
The patient and at least one family member are brought to the
treatment room. Most patients allow IV placement with parental
presence. Some patients are given an initial intramuscular (IM)
dose of ketamine, 3-5 mg/kg IM of body weight with or without
atropine, 0.02 mg/kg, as sedation for placing the IV catheter.
Once the IV 22-gauge catheter is secured, IV sedation is
started. Initially, 0.01 mg/kg of glycopyrrolate (Robinul) is given,
followed by small increments of midazolam (Versed) to induce
amnesia and anxiolysis and prevent unpleasant dreaming and
emergence phenomena from ketamine. Doses of midazolam
vary with age, weight, and level of anxiety, for example, 0.25 mg
for a 1-year-old versus 11 mg for a 10-year-old child. Ketamine
is started, usually with a small bolus followed by an infusion.
The typical initial bolus is usually up to about 1-2 mg/kg, some-
times in increments. This is followed by ketamine infusion
titrated to effect. The dose range for infusion is typically between
20 and 200 mcg/kg/min, using higher rates initially and lower
rates as the procedure progresses. The infusion is stopped
shortly before or at the conclusion of the procedure. The level of
sedation varies among patients, with most patients calm and
quiet on this regimen.
Some patients talk and move during the procedure. If
patients move excessively or begin to cry, the rate of ketamine
Gaseous Anesthesia
Nitrous oxide (N
2
O) is a sweet-smelling, nonexplosive gas
with low anesthetic potency. It is administered with at least
30% oxygen (O
2
) to prevent hypoxia. N
2
O also has good anal-
gesic properties and thus is useful as the sole analgesic agent
for brief procedures. Its safety and efficacy have been well doc-
umented in numerous studies (42,43,102-105).
Anesthesia is usually given initially at a flow rate of 6 L/min
N
2
O and 6 L/min O
2
. After approximately 1 minute, the O
2
and N
2
O flows are reduced to 3 L/min. Patients usually experi-
ence some lightheadedness and relaxation after appro-
ximately 2-3 minutes. Patients usually report a tingling
sensation of the toes or fingers. We typically use “talkathesia”
during N
2
O use to facilitate the anesthetic state. N
2
O sedation
is a helpful method for calming both children and adults
and has been extremely safe in approximately 3000 pediatric
procedures (43).
N
2
O is 35 times more soluble in blood than nitrogen. There-
fore, at the end of the procedure, it is important to wash out all
alveolar N
2
O. To avoid diffusion hypoxia, we discontinue the
N
2
O flow and ventilate the patient for 1 minute with 100% O
2
after the procedure has concluded.
Complications from N
2
O anesthesia use are limited. The
most common adverse effect is postoperative nausea and vom-
iting occurring in up to 15% of patients (44). A more serious
complication from N
2
O use is fire. Gauze is capable of igniting
when the FLPDL is used at 7 J/cm
2
in the presence of 100% O
2
(6). Hair has also been reported to ignite in room air when
struck repeatedly at this laser energy or in the setting of 100%
O
2
(6). Anecdotal report indicates one episode of ignition of a
patient's eyebrow hair by the FLPDL during the use of nitrous
oxide/oxygen. Therefore, it is recommended to wet hair and
gauze with saline and apply saline-soaked gauze to cover the
exit ports of the nose inhalation piece.
intravenous sedation
Preoperative Preparation
A history and physical examination is recommended for each
patient. The anesthetic plan should be discussed with parent(s)