Biomedical Engineering Reference
In-Depth Information
(
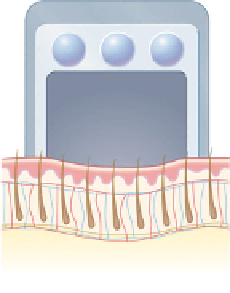
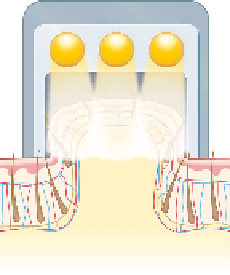
A
) Handpiece is placed on
treatment area
(
B
) Targets elevated closer to
skin's surface
Blood concentration reduced
Melanin concentration reduced
(
C
) Light applied to treatment
area
(
D
) Targets are safely and
painlessly destroyed
Figure 1.33
(
A-D
) Device that “vacuums” skin into the light path; skin is stretched and thinned, providing enhanced “relative” penetration of the beam.
100- to 430-
m
spacing (144). The tissue can recover from this fractional
injury without the widespread epidermal loss observed after
traditional resurfacing applications.
μ
m spots have been used with 250- to 500-
μ
of the beam are essentially wasted. Traveling “alone,” they carry
insuffi cient energy to cause macroscopic thermal responses in
tissue. The consequences of spot size are explained as follows.
Basically, for small beams (narrow) scattered photons are car-
ried out of the beam path after only a few scattering events.
A good analogy is a highway with exits. With a narrow highway,
any movement obliges the auto to “take” the exit, and the car
does not return to the road. On the other hand, on a superhigh-
way with many lanes, cars can move about and stay within the
original boundary of the thoroughfare. Only cars on the
extreme left and right are likely to “get” off the road. Large spots
increase the dermal-to-epidermal damage ratio as well as the
relative penetration depth. However,
absolute
epidermal dam-
age will be greater with the larger spot with the same fl uence as
the smaller spot. It follows that it is prudent to reduce the fl u-
ence by 20%, for example, if one increases the spot size between
treatment sessions in care of a PWS. Also, one should note that
for any turbid medium, even if the spot is “top hat,” there will
be an accumulation of photons near the center of the beam,
such that a greater clinical effect will often be noted at the cen-
ter of the spot. As a clinical example of the effect of spot size, we
have found for 3- versus 6-mm spots with the YAG laser that
roughly half the fl uence is required with the larger spot for leg
vein clearance. For shallow-penetrating lasers such as CO
2
and
Er where the
d
Optical Damping
Optically, replacing air (
n
= 1.0) with a higher-index medium at
the skin surface such as glass (
n
= 1.5) or sapphire (
n
= 1.7) tends
to spare the epidermis. This effect has nothing to do with heat
transfer, but rather is a consequence of optical scattering behav-
ior. At wavelengths from about 600 to 1200 nm, the majority
of light in Caucasian epidermis is actually back- and multiple-
scattered light. Indeed, the contribution of scattered light can be
almost an order of magnitude higher than that of the laser beam
itself! By providing a closer match to the skin's refractive index,
internal refl ection of the back-scattered light is greatly reduced,
decreasing the natural convergence of photons at the skin sur-
face. This version of optical epidermal sparing requires a physi-
cally thick external medium such as a thick layer of gel.
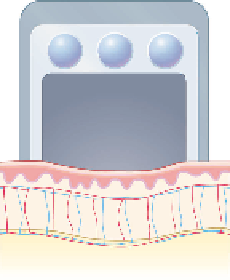
Compacting the Dermis
One can decrease the depth photons must propagate by apply-
ing pressure over the treated area. This maneuver may, for
example, decrease the relative depth of the bulb and bulge up
to 30% relative to the skin surface. Disadvantages might
include variability in the amount of pressure, such that adja-
cent treatment areas are exposed to different subsurface fl u-
ences. Also, it is unclear if compacting the dermis might alter
its scattering properties. In theory, compression should
decrease water content and improve dermal transmission (19).
Most recently fractional lasers have been confi gured with
compression optics to enhance penetration of the micro-
beams. The pressure displaces tissue water and creates a tubu-
lar light guide to decrease scattering losses (Fig. 1.34A,B)
(145,146).
spotsize, the diameter of the beam does not
intrinsically affect the tissue response. That is why equivalent
results can be obtained for skin resurfacing, using pulsed CO
2
lasers versus scanned, tightly focused CW CO
2
lasers (147).
<<
Changing Optical Properties in Real Time
One should always be aware of the changing chromophore
concentrations as a function of time during a treatment ses-
sion. One should never consider each laser-tissue interac-
tion as an independent event, but rather a cumulative process
where visual endpoints are the most important ally for the
physician. Optical properties of the skin are like the weather
(5), and one must accommodate the changes in real time.
For example, the dermal blood fraction increases after one
pass of the PDL, such that for a second pass, the skin tem-
perature will increase due to the higher
m
a
(148). A failure to
Spot Diameter
In general, the spot size should be 3-4× >
d
, as larger spots
make it more likely that photons will be scattered back into the
incident collimated beam (112). Photons that are scattered out