Biomedical Engineering Reference
In-Depth Information
manufacturers, few well-controlled peer-reviewed medical
studies are available. A study on 30 women with leg telangiecta-
sia compared treatment with 75% glucose solution sclerother-
apy without the use of compression to long-pulsed 1064-nm
Nd:YAG treatment using 100-120 J/cm
2
, 15-30 ms, and 3-mm
cooled spot (Xero, Cutera Inc., Brisbane, California, USA) and
found that sclerotherapy was less painful and led to faster clini-
cal improvement. This was signifi cant since the sclerotherapy
treatment utilized was suboptimal using no compression and a
very low potency sclerosing solution (22).
To summarize, we have found the 1064-nm, long-pulsed
Nd:YAG lasers to be benefi cial in the treatment of leg telangiec-
tasia not responsive to sclerotherapy or other lasers (Fig. 11.6).
The benefi t of using a 1064-nm laser is that its longer wavelength
can penetrate more deeply, allowing effective thermosclerosis of
vessels up to 3-4 mm in diameter. In addition, the 1064-nm
wavelength permits treatment of patients of skin types I-VI with
or without a tan, since melanin absorption is minimal. The
1064-nm, long-pulsed laser systems are not entirely without side
effects. Cutaneous burns with resulting ulceration, pigmenta-
tion, and TM have been observed with each of these systems as
parameters are being tested. The dynamically cooled 1064-nm
Nd:YAG laser appears to produce the best clinical resolution
with the least pain and adverse effects compared with other long-
pulsed 1064-nm lasers. However, sclerotherapy still provides bet-
ter results in fewer treatments, is associated with less pain, and
has comparable adverse effects with lasers. Thus, the reader
should evaluate the latest studies to ensure ideal results.
In a similar “vein,” enhanced effi cacy of treatment may occur
when combining sclerotherapy with lasers or IPL. This tech-
nique is not new and was even reported approximately 30 years
ago by the Italian vascular surgeon Leonardo Corcos, who used
the argon laser to spot-weld telangiectasia so the sclerosing solu-
tion could have a prolonged contact with the vessel wall (24).
This combination technique also gives the patient the opportu-
nity to experience “laser” treatment, which is perceived as more
advanced than merely injecting a solution into a vein. The opti-
mal effi cacy in treating common leg telangiectasia uses sclero-
therapy to treat the feeding venous system and a laser or IPL to
seal off superfi cial vessels, thus preventing extravasation with
resulting pigmentation, recanalization, and TM.
So, is there a single laser that can adequately treat leg veins?
The answer is yes and no. Yes, lasers are now available with
pulse durations optimized to treat blood vessels of various
sizes. One can select virtually any wavelength from 532 to
1064 nm, as well as a broad spectrum of IPL. It has been dem-
onstrated that any wavelength can be used effectively as long as
the pulse duration matches the diameter of the vessel and an
appropriate fl uence is utilized. This also assumes that the epi-
dermis will be protected from nonspecifi c thermal effects by a
variety of cooling and pulsing scenarios. One can cool the skin
directly with a contact probe before and after the laser pulse or
through a sapphire window before, during, and after the laser
pulse. Cooling can also be given dynamically with a cryogen
spray before, during, or after the laser pulse. Most patients pre-
fer dynamic cooling as providing the highest degree of pain
control. Contact cooling is unpredictable in adequately cool-
ing the epidermis; unless optimal techniques are used, epider-
mal burns will occur.
However, the answer is also no, as presently available lasers
still require skillful use for safe and effective treatment (Figs. 11.7
and 11.8). The ideal laser of the future (25) will have a built-in
thermal sensor to detect both epidermal and vascular heating.
This will automatically regulate the fl uence so that the vessel
is completely thermocoagulated while cooling the epidermis to
maintain its temperature at that of one below a damaging
threshold. Even better would be an infrared sensor that would
determine the location of feeding dermal vessels so that they
conclusions
As sclerotherapy treatment is relatively cost-effective com-
pared with laser or IPL treatment, when is it appropriate to use
this advanced therapy? Obviously, needle-phobic patients will
tolerate this technology even though the pain from lasers and
IPL is more intense than that of sclerotherapy with all but
hypertonic solutions. Patients who are prone to TM are also
appropriate candidates. Finally, patients who have vessels that
are resistant to sclerotherapy are excellent candidates. Effi cacy
of 75% clearance with two to three IPL treatments occurred in
sclerotherapy-resistant vessels (23).
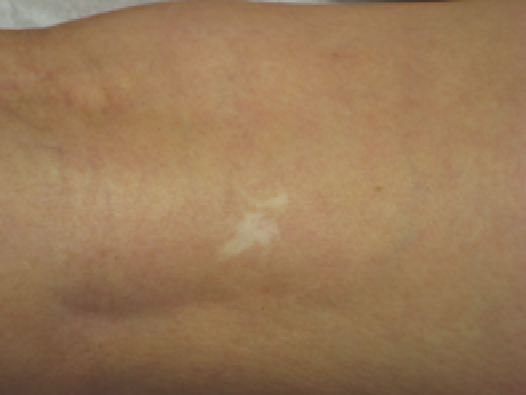
Figure 11.7
Hypopigmented scar 1 year after treatment of leg telangiectasia by
a nurse in a plastic surgeon's offi ce with an 800-nm diode laser.
Figure 11.8
Hyperpigmentation 9 months after treatment of leg telangiectasia
by a nurse at a medical spa with a long-pulsed alexandrite laser.