Biomedical Engineering Reference
In-Depth Information
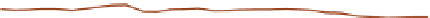
Skin and blood absorption,
scattering and attenuation data
10000
1000
Dermis absorption
Oxyhemoglobin absorption
Deoxyhemoglobin absorption
Dermis scattering
Effective attenuation
100
10
1
0
400
500
600
700
800
900
1000
Wavelength (nm)
Figure 11.1
Coefficient of blood relative to dermis.
Source
: Courtesy of ESC Medical, Inc.; redrawn from Ref. 28.
with appropriate fl uences, pulse durations, and epidermal
cooling, the thermal effects of lasers and IPL present minimal
infl ammatory response compared with chemical irritation of
the vessel wall through sclerotherapy. An understanding of the
appropriate target vessel for each laser and/or IPL is important
so that treatment is tailored to the appropriate target. Telangi-
ectasia arises mostly from reticular veins. Therefore, the single
most important concept for the treating physician is that feed-
ing reticular veins must be treated completely before treating
telangiectasia. This minimizes adverse sequelae and enhances
therapeutic results. When no apparent connection exists
between deep collecting and reticular vessels, telangiectasia
may arise from a terminal arteriole or arteriovenous anasto-
mosis (8). In this latter scenario, the telangiectasia may be
treated without consideration of underlying forces of hydro-
static pressure. Failure to treat “feeding” reticular veins and
short follow-up periods after the use of lasers may give infl ated
values to the success of laser treatment (9). This chapter
reviews and evaluates the use of these nonspecifi c and specifi c
laser and light systems in the treatment of leg venules and
telangiectasias.
form of epidermal cooling. A number of different laser and
IPL systems have been developed toward this end, as discussed
in subsequent sections. In addition to the information pre-
sented in the following sections, the reader is encouraged to
refer to an excellent summary of various laser treatments for
leg veins by Kunishige et al. (3).
krypton triphosphate
and frequency-doubled n
nm)
Modulated krypton triphosphate (KTP) lasers have been
reported to be effective in removing leg telangiectasia, using
pulse durations between 1 and 50 ms. The 532-nm wavelength
is one of the hemoglobin absorption peaks. Although this
wavelength does not penetrate deeply into the dermis (about
0.75 mm), relatively specifi c damage can occur in the vascular
target by selection of an optimal pulse duration, enlargement
of the spot size, and addition of epidermal cooling. Effective
results have been achieved by tracing vessels with a 1-mm pro-
jected spot. Typically, the laser is moved between adjacent
1-mm spots with vessels traced at 5-10 mm/second. Immedi-
ately after the laser exposure, the epidermis is blanched.
Lengthening of the pulse duration to match the diameter of
the vessel is attempted to optimize treatment. Usually, more
than one treatment is necessary for maximum vessel improve-
ment, with only rare reports of 100% resolution of the leg vein.
Effi cacy is technique dependent, with excellent results achiev-
able. Patients need to be informed of the possibility of pro-
longed pigmentation at an incidence similar to that with
sclerotherapy, as well as temporary blistering and hypopig-
mentation that is predominantly caused by epidermal damage
in pigmented skin (type III or above, especially when tanned)
(Fig. 11.2).
d
:yag
(
532
laser treatment of leg telangiectasia
Various lasers have been used in an effort to enhance clinical
effi cacy and to minimize the adverse sequelae of telangiectasia
treatment. (Table 11.1) Unfortunately, most have also been
associated with adverse responses far in excess of those associ-
ated with sclerotherapy. This is related to both the nonspecifi c-
ity of the laser used and the lack of treatment of hydrostatic
pressure from the “feeding” venous system. The optimal light
source would have a wavelength specifi c for the vessel treated
and would be able to penetrate to the depth of the vessel
through its entire diameter. This wavelength has been pro-
posed to be between 600 and 900 nm. Ideally, a light source
should have a pulse duration that would allow the light energy
to build up in the target vessel so that its entire diameter is
thermocoagulated. Optimal pulse durations have been calcu-
lated for various diameter blood vessels (Table 11.2). During
the process of delivering a suffi cient packet of energy to ther-
mocoagulate the target vessel, the overlying epidermis and
perivascular tissue should be unharmed. This requires some
flashlamp-pulsed dye laser
nm)
The PDL has been demonstrated to be highly effective in treat-
ing cutaneous vascular lesions consisting of very small vessels,
including PWSs, hemangiomas, and facial telangiectasia. The
depth of vascular damage is estimated to be 1.5 mm at 585 nm
and 15-20 µm deeper at 595 nm. Therefore, penetration to the
typical depth of superfi cial leg telangiectasia may be achieved.
However, telangiectasia over the lower extremities has not
(
585 or 595