Biomedical Engineering Reference
In-Depth Information
fraction of its energy is invested in heating rather than ablating
tissue (6). Consequently, the CO
2
laser produces relatively large
residual thermal damage zones and causes signifi cant desicca-
tion of the target tissue after only a few passes. With each sub-
sequent pass the amount of vaporized tissue decreases while
thermal damage increases, and a “plateau” of ablation is
typically reached after the fourth pass. Nonspecifi c thermal
damage has a negative impact not only on the CO
2
laser's abla-
tive capacity but also on its side effect profi le. The relatively
large thermally induced residual zone of necrosis (up to
150
m) left behind by the CO
2
laser is one of the main factors
contributing to its adverse sequelae, including prolonged ery-
thema, postoperative pain, delayed healing, infection, and
scarring.
Given the complications encountered with CO
2
laser resurfac-
ing, clinicians began looking for an alternative ablative resurfac-
ing laser. Ideally, this would be a laser system capable of carrying
out considerably greater ablation with a signifi cantly reduced
residual zone of nonspecifi c thermal damage. The arrival of the
Er:YAG laser in the mid-1990s made available to clinicians a laser
system, which successfully met both of these “ideal” criteria.
With a wavelength of 2940 nm (near-infrared light) and a
coeffi cient of absorption for water that is 16 times greater than
that of the CO
2
laser (7), the energy absorbed by the Er:YAG
laser is in a much thinner layer of tissue (1
μ
Estimated resurfacing depth of various
modalities in a porcine model
2500
Clinical resurfacing depth
Baker's phenol
Dermabrasion
35% TCA
2400
450 mJ/pulse
350 mJ/pulse
250 mJ/pulse
150 mJ/pulse
2300
1200
Reticular
dermis
1100
1000
Deep resurfacing
900
800
m) than the CO
2
laser's irradiation. Its greater affi nity for water (16 times
greater than that of the CO
2
laser) allows the Er:YAG laser to
carry out precise and effi cient ablation of tissue with very little
scattering of the laser beam and minimal residual thermal
damage. Short-pulsed (350
μ
700
600
Medium deep resurfacing
500
400
300
μ
s) Er:YAG lasers reliably ablate
Papillary
dermis
Epidermis
200
5-15
m of tissue per pass at a fl uence of 5 J/cm
2
, producing a
residual zone of thermal damage not exceeding 15
μ
100
0
μ
m (5,8). In
Superficial resurfacing
contrast, the CO
2
laser produces 20-60
μ
m of tissue ablation
I
II
III
and up to 150
m of residual thermal damage per pass (9).
Moreover, given the limited zone of residual thermal damage
produced by the Er:YAG laser, tissue desiccation does not sig-
nifi cantly increase with each subsequent pass and the ablation
μ
Number of laser passes
Figure 6.1
Varying pulse energies and passes of UltraPulse CO
2
laser resulted
in resurfacing depths comparable with those of TCA peels or dermabrasion
but not those of phenol peels.
Abbreviation
: TCA, trichloroacetic acid.
(
A
)
(
B
)
(
C
)
(
D
)
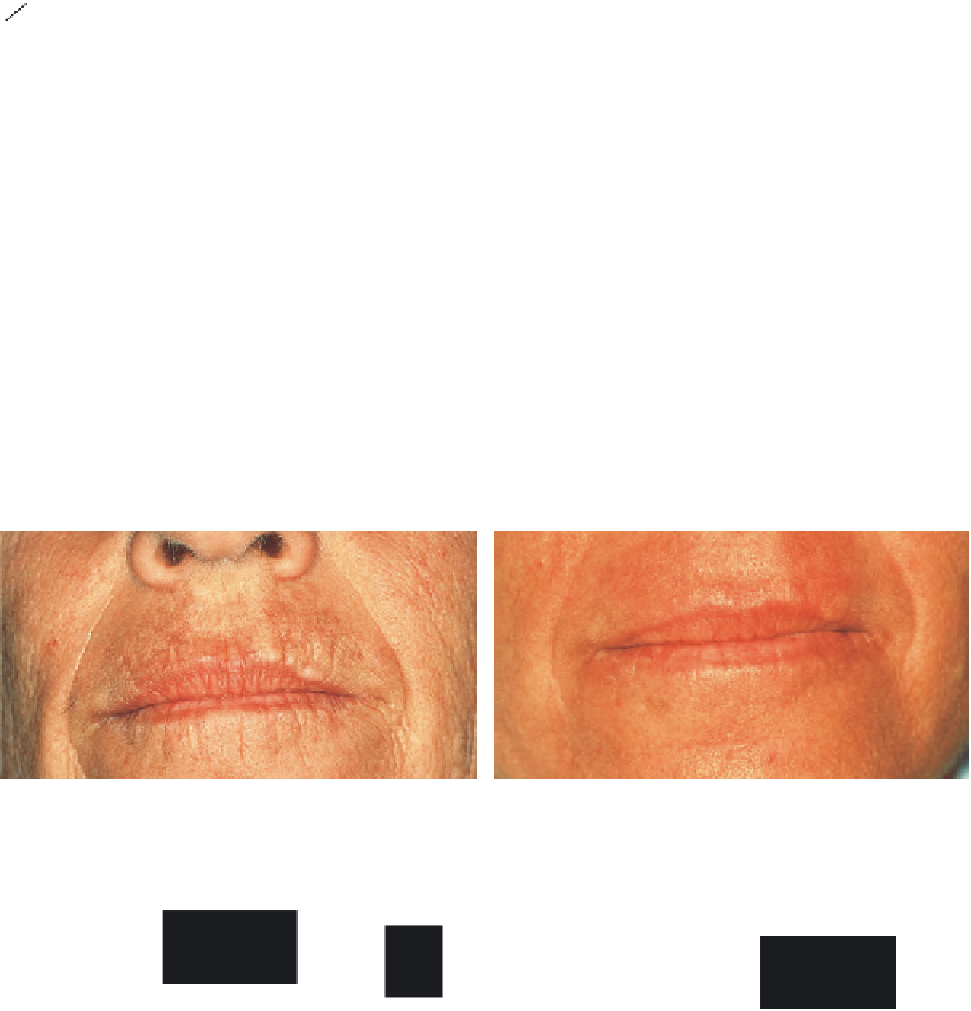
Figure 6.2
Signifi cant perioral photodamage (class III, level 7) (
A
) before treatment; (
B
) 6 months postoperatively, dramatic improvement, with photodamage now
rated class I, level 2; (
C
) periorbital photodamage (class II, level 6) before treatment; (
D
) 9 months postoperatively, signifi cant improvement, with photodamage
now rated class I, level 3.