Biomedical Engineering Reference
In-Depth Information
examination after several weeks revealed differentiated
intestinal epithelium lining of the tubes and this epi-
thelium appeared to secrete mucus (
Vacanti
et al.
, 1988
).
Furthermore, intestinal epithelial organoid units trans-
planted on porous biodegradable polymer tubes have
been shown to vascularize and to regenerate into com-
plex tissue resembling small intestine (
Kim
et al.
, 1999
),
and successful anastomosis between tissue-engineered
intestine and native small bowel has been performed
(
Fig. 7.1.2-3
;
Kaihara
et al.
, 1999
). Finally, Perez
et al.
demonstrated that tissue-engineered small intestine is
capable of developing a mature immunocyte population
and that mucosal exposure to luminal stimuli is critical to
this development (
Perez
et al.
, 2002
). Despite these
promising findings, the regeneration of the muscle layer
seems to be a major problem. Autologous mesenchymal
stem cells seeded onto a collagen sponge graft induced
only a transient distribution of cells positive for a-smooth
muscle actin (
Hori
et al.
, 2002
).
Tubular structures have also been used in kidney re-
placement. As a first step toward creating a bioartificial
kidney, renal tubular cells have been grown on acrylonitrile-
vinyl chloride copolymers or microporous cellulose ni-
trate membranes.
In vitro,
these cells transported glucose
and tetraethylammonium cation in the presence of
a hemofiltrate of uremic patients (
Uludag
et al.
, 1990
).
In a further attempt to create bioartificial renal tubule,
renal epithelial cells have been grown on hollow fibers
and formed an intact monolayer exhibiting functional
active transport capabilities (
MacKay
et al.
, 1998
). Fi-
nally, an extracorporeal device was developed using
a standard hemofiltration cartridge containing renal
tubule cells (
Humes
et al.
, 1999
;
Nikolovski
et al.
, 1999
).
The pore size of the hollow fibers allows the membranes
to act as scaffolds for the cells and as an immunopro-
tective barrier.
In vitro
and
in vivo
studies have shown
that the cells keep differentiated active transport, dif-
ferentiated metabolic transport, and important endo-
crine processes (
Humes
et al.
, 2002
, 2003).
For replacement of urether, urothelial cells were
seeded onto degradable PGA tubes and implanted in
rats and rabbits resulting in two or three layers of
urothelial cell lining (
Atala
et al.
, 1992
). More recently,
an acellular collagen matrix from bladder submucosa
seeded with cells from urethral tissue was also suc-
cessfully used for tubularized replacement in the rabbit.
In contrast, unseeded matrices lead to poor tissue de-
velopment (
de Filippo
et al.
, 2002
). A neo-bladder has
been created from urothelial and smooth muscle cells
in vitro
and after implantation in the animal, functional
evaluation for up to 11 months has demonstrated
a normal capacity to retain urine, normal elastic prop-
erties, and normal histologic architecture (
Oberpenning
et al.
, 1999
).
Mesoderm
Cartilage
More than 1 million surgical procedures in the United
States each year involve cartilage replacement. Current
therapies include cartilage transplantation and implan-
tation of artificial polymer or metal prostheses. Un-
fortunately, donor tissue is limited and artificial implants
may result in infection and adhesive breakdown at the
host-prosthesis interface. Finally, a prosthesis cannot
adapt in response to environmental stresses as does car-
tilage (
Mow
et al.
, 1992
). The need for improved treat-
ments has motivated research aiming at creating new
cartilage that is based on collagen-glycosaminglycan
templates (
Stone
et al.
, 1990
), isolated chondrocytes
(
Grande
et al.
, 1989
), and chondrocytes attached to
natural or synthetic polymers (
Cancedda
et al.
,2003
;
Va c a n t i
et al.
,1991
;
Wa k i ta ni
et al.
,1989
). It is critical
that the cartilage transplant have an appropriate thickness
and attachment to be mechanically functional. Chon-
drocytes grown in agarose gel culture have been shown to
produce tissues with stiffness and compressibility com-
parable to those of articular cartilage (Freed
et al.
, 1993).
The use of bioreactors for cultivating chondrocytes on
polymer scaffolds
in vitro
enables nutrients to penetrate
the center of this nonvascularized tissue, leading to rel-
atively strong and thick (up to 0.5 cm) implants
(
Buschmann
et al.
, 1992
). Moreover, it has been shown
that the hydrodynamic conditions in tissue-culture bio-
reactors can modulate the composition, morphology,
mechanical properties, and electromechanical function
of engineered cartilage (
Vunjak-Novakovic
et al.
, 1999
).
In other studies, chondrocytes were seeded onto PGA
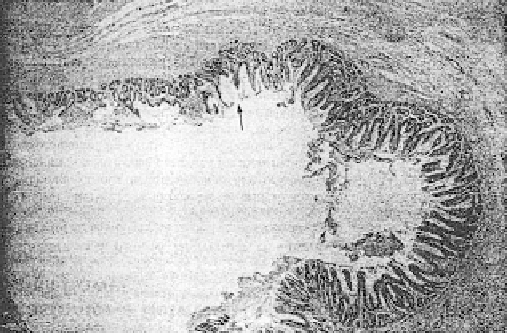
Fig. 7.1.2-3 Histology of a tissue-engineered intestine 10 weeks
after implantation characterized by crypt villus structures. Arrow
indicates anastomosis site; left site of the arrow is tissue-
engineered intestine and right is native small bowel. (Reprinted
with permission from Kaihara, S., et al., 1999. Transpl. Proc.
31: 661-662.)