Biomedical Engineering Reference
In-Depth Information
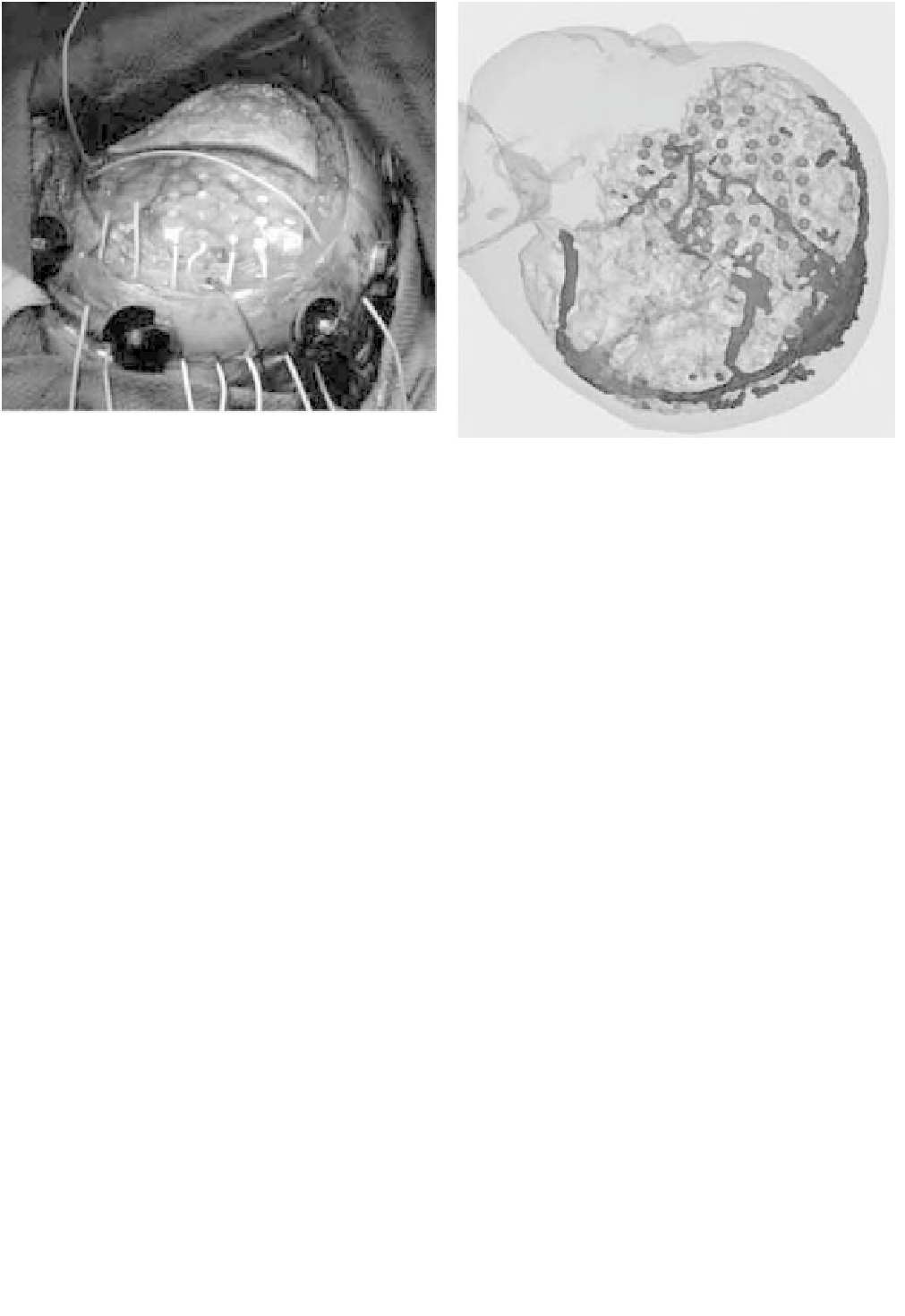
Figure 6.5-9 Grid of electrodes placed on cortical surface. Location of grid points overlaid on MR reconstruction, with focal area
highlighted.
One example of the effectiveness of the system is il-
lustrated by the following study. Twenty patients with
low-grade gliomas underwent surgery with the system.
The pathologies included 10 low-grade astrocytomas
(grades I, II out of IV), 7 oligoastrocytomas (without
anaplastic features), and 3 oligodendrogliomas. Thirteen
patients underwent cortical mapping, including 7 who
underwent speech and motor mapping, 2 motor alone,
1 speech alone, and 3 motor and sensory. This cortical
mapping was then registered with the structural MRI
model and used to provide guidance to the surgeon. In
these cases, 31% had a subtotal resection; the remainder
had total resection. One patient exhibited temporary
left-sided weakness. Cortical mapping had represented
the sensory cortex diffusely behind this patient's gross
tumor. The postoperative weakness was temporary and
was thought to be due to swelling. One patient showed
a mild, left upper extremity proprioreceptive deficit,
which was due to a vascular accident on postoperative
day 1. The remaining patients were neurologically intact
following the procedure.
In addition to the tumor resection cases, we have also
used the system in 10 pediatric epilepsy cases
[4]
. In the
first stage of this two-stage surgery, the patient's cortex is
exposed and a grid of electrical pickups is placed on the
cortical surface. A lead from each pickup is threaded out
through the skin for future monitoring. In addition to
registering the MRI model of the patient to his/her po-
sition, the location of each electrical contact is recorded
and transformed to MRI co ordinates. The patient is then
closed up and monitored for several days. During any
seizure event, the activity from each cortical probe is
monitored, and transformed to the MRI model. This
enables the surgeon to isolate potential foci in MRI co-
ordinates. During a second surgical procedure, the aug-
mented MRI model is reregistered to the patient and the
locations of the hypothesized foci are presented to the
surgeon for navigational guidance. An example of this is
shown in
Fig. 6.5-9
.
To see the range of cases handled by our system, we
encourage readers to visit theWeb site
http://splweb.bwh
.
harvard.edu:8000/pages/comonth.html, which shows se-
lected cases with descriptions of the use and impact of the
navigation system on the case.
6.5.6 Summary
We have described an image-guided neurosurgery
system, now in use in the operating room. The system
achieves high positional accuracy with a simple, efficient
interface that interferes little with normal operating
room procedures, while supporting a wide range of cases.
Qualitative assessment of the system in the operating
room indicates strong potential. In addition to
performing quantitative testing on the system, we are
also extending its capabilities by integrating a screw-
based head tracking system and improved visualization
capabilities.