Biomedical Engineering Reference
In-Depth Information
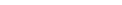
Electrical contact
EYEPIECE
Light Guide Tube
Air/Water Valve
Suction Valve
Up/Down
Angulation
Control
Right/Left
Angulation
Control
Channel Opening
DISTAL END
Flexible Insertion Tube
Light Guide
LIGHT GUIDE CONNECTOR
SECTION
Distal End
Venting Connection
Suction Connector
Objective Lens
Instrument
Channel
Bending
Section
Air/Water
Nozzle
Water Bottle
Air/Pipe
Light Guide
Figure 6.2-22 Flexible endoscope for looking at gastrointestinal tract without surgery.
bleeding. Endoscopes for this purpose cost around
$15,000 and typically have lifetimes of about 3000 uses.
The endoscope can improve its image quality and get
smaller to give the patient more comfort. Furthermore,
the methods of cleaning and sterilizing the reusable in-
struments are complicated and time consuming. At-
tempts to make semidisposable endoscopes have not had
great success. Patients sometimes avoid the uncomfort-
able procedure because it requires sedation and/or local
anesthetic. In addition, endoscopes cannot reach all parts
of the small intestine. However, making endoscopes that
can go wireless would allow doctors to take endoscopes
where they could not go before and could make patients
more comfortable. An endoscope is illustrated in
Figure
6.2-22
.
impressive results, a report released by the Institute of
Medicine concludes that such technologies will only play
a supporting role to film-screen mammography. Film
mammography is the gold standard for screening for
breast cancer and the technology against which all other
technologies will be benchmarked.
Presently, abnormalities and lesions are discovered
either by physical examination or by screening mam-
mography, a task performed by a radiologist. Once
identified, the abnormality must be diagnosed as benign
or malignant by using other imaging technologies such as
ultrasound or a biopsy and microscopic examination. The
true tumors are biochemically characterized and cate-
gorized (staged) according to size and how much they
have spread. The system is not flawless. It misses up to
20% of the tumors and many of those are found later to
be benign.
Screening tools have to be highly sensitive, identify-
ing as correctly as possible those tumors that could be
malignant. Diagnostic tools must have a great specifi-
city in order to really catch those tumors that are
malignant.
Digital mammography (
Figure 6.2-23
) is the new
technology most certain to see clinical use. With its high
spatial resolution, mammography requires very small
pixels and a high signal-to-noise ratio. The digital version
of the technology has superior dynamic range and line-
arity compared to film, leading to a much better contrast
resolution. It also allows the images to be manipulated
and analyzed with software. This approach may lead to
the discovery of more subtle features indicative of cancer
6.2.7 Digital x rays
Breast cancer remains a leading cause of cancer deaths in
the world (50,000
þ
a year in the United States alone).
Better diagnosis and treatment of breast cancer have
noticeably improved the outcome of the disease, re-
ducing death rates over the last decade by about 2% per
year in the United States. A great deal of that success is
due to earlier detection by the standard breast imaging
technology, film-screen x-ray mammography.
The variety and sophistication of imaging technologies
have increased greatly, encompassing everything from
optical laser imaging to digital mammography. While
these new technologies (see
Table 6.2-5
) have shown