Biomedical Engineering Reference
In-Depth Information
4.0
3.5
3.0
2.5
2.0
1.5
1.0
0.5
Polyester core (PBT)
Polypropylene core (Type 1)
Polypropylene core (Type 2)
Expanded PTFE
0.0
-0.5
0
1
2
3
4
5
6
7
8
9
Weeks
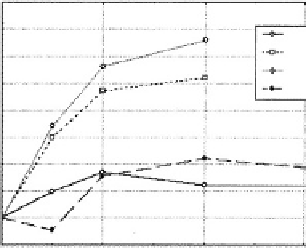
Fig. 3.2.4-5 Creep characteristics of various graft materials
(Weinberg,1998).
A
Figure 3.2.4-5
demonstrates the creep characteristics of
grafts fabricated from expanded polytetrafluoroethylene
(e-PTFE), polyester, and a BCF containing PP yarns. In
the case of the first BCF design (see later section), the PP
was used as the nonabsorbable core material and the main
structural component of the fiber.
Figure 3.2.4-5
repre-
sents the outer diameter of a series of pressurized graft
materials as a function of time. Classical graft materials
such as PET and e-PTFE show no creep over time,
whereas the PP-based materials continue to creep over
time, making them unacceptable for long-term vascular
implants. However, in other applications such as for
hernia repair meshes and sutures, PP has been used very
successfully. It should be noted that in the second-gen-
eration BCF design, the core material was changed to
poly(butylene terephthalate) (
King
et al.
, 2000
).
B
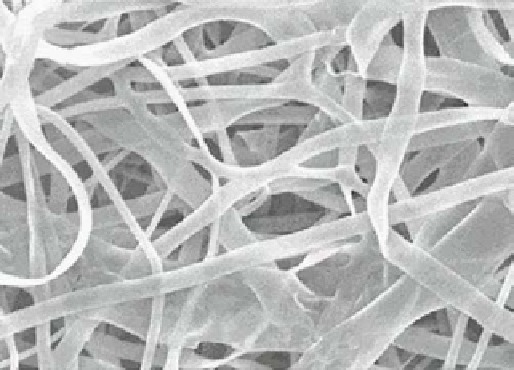
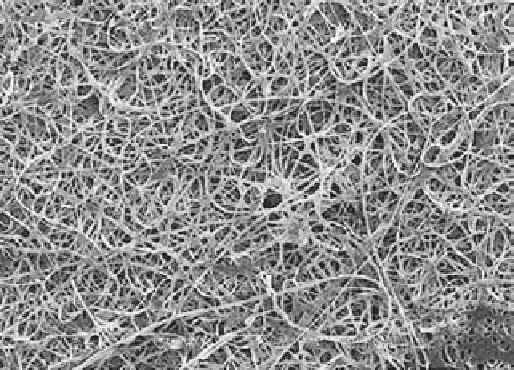
Fig. 3.2.4-4 Electrospun fibers from biomimetic-elastin peptide.
Absorbable synthetic fibers
Another series of synthetic fibers used in clinical appli-
cations are constructed from polymers that are designed
to be absorbed over time when placed in the body. They
classically have been used as sutures, but have also been
used experimentally for neurological, vascular graft, and
tissue scaffold applications.
Table 3.2.4-3
is a list of
bioabsorbable polymers that have been used in the past
to fabricate medical devices. When in contact with the
body, these polymers degrade either by hydrolysis or by
enzymatic degradation into nontoxic by products. They
break down or degrade either through an erosion process
that starts on the exterior surface of the fiber and con-
tinues until the fiber has been totally absorbed, or by a bulk
erosion mechanism in which the process is autocatalytic
and starts in the center of the fiber. Caution should be
exercised when using these types of materials. In vascular
applications, the risk of distal embolization to the micro-
vasculature may occur if small pieces of the polymer break
off during the erosion or absorption process.
Escherichia coli.
The protein has been electrospun into
fibers with diameters varying between 3 nm and 200 nm
(
Huang
et al.
, 2000
)(
Fig. 3.2.4-4
).
Polymer and fiber selection
When deciding on a polymer and fiber structure to be
incorporated into the construction of a medical fabric,
careful consideration of the end use is necessary. Issues
such as the duration of body contact, device mechanical
properties, fabrication restrictions, and sterilization
methods must be considered. To illustrate this point,
PP has been successfully used in many implantable ap-
plications such as a support mesh for hernia repair. Ex-
perience has shown that PP has excellent characteristics
in terms of tissue compatibility and can be fabricated into
a graft material with adequate mechanical strength. A
critical question remaining is whether the graft will
remain
stable
and
survive
as
a
long-term
implant.