Biomedical Engineering Reference
In-Depth Information
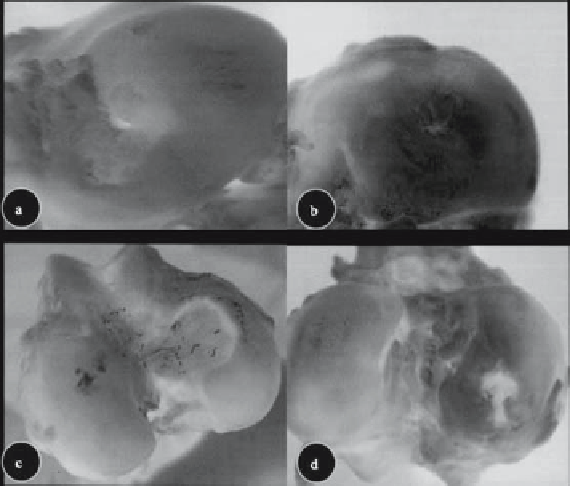
Figure 1.3.
Bone marrow-derived mesenchymal stem cells (BM-MSCs) form new articular cartilage in vivo. At 12 weeks post-
operation, the defects in the BM-MSC group were mostly repaired with tissue-engineered cartilage, resulting in a relatively smooth
and consistent joint surface (A). At 24 weeks postoperation, the regenerated area was covered by smooth, consistent hyaline tissue
that was indistinguishable from the surrounding normal cartilage (B). The defects in control group 1 were partially repaired with
fibrous tissue, leaving some depression in the defect areas (C). In control group 2, a thin layer of red, irregular tissue surfacing
the defects can be seen, and cracks on the surrounding normal cartilage are obvious (D). Reprinted from Guo et al. [36]. Copyright
2004, with permission from the European Association for Cranio-Maxillofacial Surgery.
compression and shear moduli increase after
28
(PLGA) scaffolds supported cartilage formation
by BM-MSCs transplanted into rabbit patellar
defects [
days of culture, but this does not occur when
they are loaded onto hydrogel-based matrices
[
]. Stem cells derived from allogenic
rabbit adipose tissue, when delivered in a
fi brin matrix, formed cartilage in an articular
condyle defect that, on histological examina-
tion, appeared to have become integrated with
the surrounding host tissue [
114
].
The effi cacy of stem-cell chondrogenesis is
model-dependent. Direct addition of stem cells
to articular cartilage defects in rabbit and dog
condyles generated tissue that was histologi-
cally comparable to native tissue [
11
]. However, the
new tissue became degraded after
82
]. However,
both bone-marrow-derived and adipose-
derived cartilage displayed less strength and
elasticity than native cartilage. Direct addition
of BM-MSCs in a caprine osteoarthritis model
reduced cartilage loss and induced cartilage
regeneration [
1
12
weeks.
] recapitulated the
host microenvironment and had greater long-
term success. They utilized a two-layered
matrix composed of a bottom layer of inject-
able calcium phosphate and a top layer of hyal-
uronan and found that by
Gao and colleagues [
32
]. Cells derived from autolo-
gous rabbit bone marrow were able to regener-
ate a femoral condyle defect when loaded in a
collagen gel [
80
weeks the defects
had become fi lled with a stratifi ed osteochon-
dral tissue that was integrated into the sur-
rounding tissue.
Alhadlaq and colleagues created a composite
human articular condyle by predifferentiating
BM-MSCs along the chondrogenic or osteo-
genic pathways and then loading the cells into
photopolymerization gels [
12
]. Twenty-four weeks after
transplantation, the reparative tissue from the
BM-MSCs was stiffer and less compliant than
the tissue derived from the empty defects, but it
was less stiff and more compliant than normal
cartilage [
117
117
]. Poly(lactic-co-glycolic acid)
3
]. The mold was