Biomedical Engineering Reference
In-Depth Information
extraction [
] indicate that the
degree of resorption is a function of gender
and age. Further, because the tooth extraction
site involves both soft and hard tissues, it
represents a unique situation for evaluating
bone healing and regenerative devices and
molecules.
The healing of an extraction site is affected
by events in two regions of the healing site: the
socket space where the root was located and the
residual alveolar bone that supported the tooth.
Histologic evaluation of the healing tooth
socket has shown that the resultant bone for-
mation fi lls most of the space. Initial clot for-
mation is followed by cellular infi ltration with
the formation of highly vascularized granula-
tion tissue. Osteoid becomes evident
30
,
32
,
48
,
69
7
to
14
days after extraction, and by
days the major-
ity of the socket space has become fi lled with
mineralized tissue [
30
]. Even though a corti-
cal “bridge” covers the coronal aspect of the
socket space, the newly formed alveolar bone
within the socket continues to remodel, with an
increasing percentage of marrow space devel-
oping over time. Furthermore, residual tissues
from the disrupted periodontal ligament fol-
lowing tooth extraction appear to have little
effect on this healing process [
1
,
12
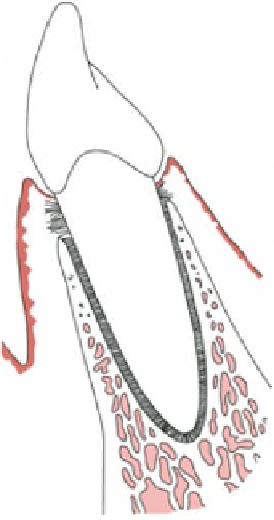
Figure 9.1.
Schematic cross-sectional representation of the
tooth-supporting tissues of the periodontium.
].
The second region involved in the extraction
site is the retained alveolar bone that previ-
ously supported the tooth. Numerous studies
have demonstrated that signifi cant dimen-
sional losses, involving as much as
12
through the mandible, innervating and supply-
ing blood to the lips and face. As a result, only
a limited amount of vertical bone is left. When
teeth are lost from the maxilla, the sinuses
located above the roots of the back teeth enlarge
and thus come close to the remaining alveolar
ridge crest. This also weakens denture
support.
Tooth replacement has been revolutionized
by dental implant therapy, which over the last
three decades has become the optimal form of
tooth replacement [
% of the
buccolingual dimension of the alveolar ridge,
occur within the fi rst
50
months of healing.
This dimensional change can amount to
3
to
4
5
to
7
mm of horizontal bone loss and can have a
great impact on subsequent dental implant
therapy [
]. The patterns of resorp-
tion of the residual bone are unique, with
greater resorption occurring along the facial
than the lingual aspect of the extraction site
[
3
,
13
,
49
,
56
]. Implants are endosse-
ous titanium screw devices that, after careful
preparation of the bone, are screwed into the
bone tissue to a depth that ranges from
15
12
mm. The procedure is successful in more than
90
8
to
]. This may be because the facial alveolar wall
is thinner than the lingual aspect and may
therefore be more susceptible to losses of ridge
height and width that occur in the course of
bone remodeling during the healing process.
Recent attempts to modify the relatively
extensive resorption of bone that occurs after
tooth extraction have included placement of a
dental implant into the extraction site immedi-
ately after tooth removal and bone grafting of
the sites following the principles of guided
bone regeneration (GBR), as will be discussed.
2
% of cases. Moreover, a small number of
implants can replace many teeth. Implant
therapy depends on bone dimensions adequate
to allow placing the implant in the bone. Fol-
lowing tooth extraction, alveolar bone under-
goes remodeling typical of tissue injury and
infl ammation. Some systemic interactions may
impact upon the remodeling process. Studies of
the relationship between bone mineral density
(BMD) and alveolar ridge resorption following