Biology Reference
In-Depth Information
dead
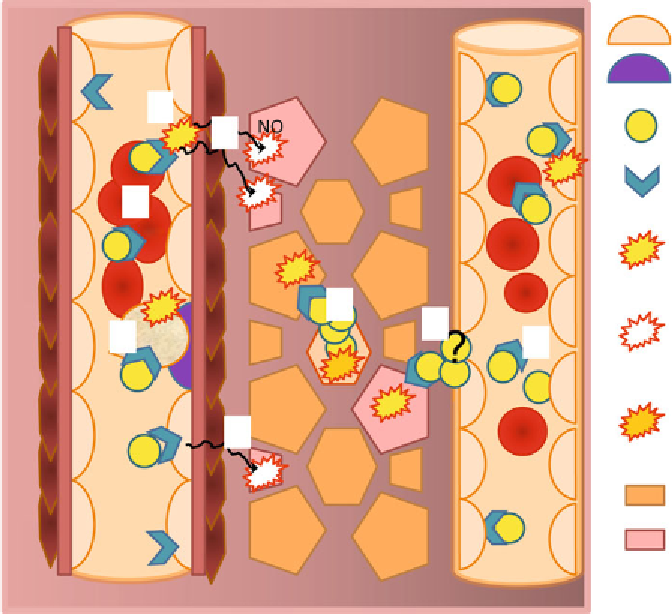
Fig. 2
Schematic representation of the multiple putative cytoprotective effects of Epo in non-erythropoietic
tissues. Interaction of blood-borne Epo with heterodimeric Epo receptors on endothelial cells activates the
PI3K-Akt pathway (
1
) leading to NO production by eNOS and its translocation to the periphery where it induces
cytoprotective effects (
2
). Another second messenger known to be released by endothelial cells upon their
stimulation with Epo is endothelin 1 (ET-1) which also elicits protective effects in peripheral cells (
3
). Further
targets of circulating Epo are blood cells, including red blood cells and macrophages. Similar to endothelial
cells, Epo binding to red blood cells triggers production of NO by eNOS (
4
). Endothelial precursor cells (EPCs)
are very sensitive to Epo. Epo controls their number, recruitment to the site of injury, homing, and the quality
of resulting mature endothelial cells (
5
). Peripheral cells were shown to respond to Epo stimulation directly.
Blood vessels are largely impermeable for Epo when undamaged. However the blood-tissue barrier is less tight
in capillaries and although leakage of Epo from the capillary system into the peripheral tissue has never been
demonstrated convincingly, it cannot be excluded (
6
). Alternatively, peripheral cells may produce their own
Epo. Indeed induction of Epo expression has been demonstrated in hypoxic brain and heart. Thus once pro-
duced the cytokine is released causing autocrine and paracrine effects (
7
). Action of Epo is transient and the
cytokine is internalized and degraded upon binding to the receptor. Free Epo pools in the plasma may also be
regulated by sequestration of the circulating soluble Epo receptor (
8
). For more details of these mechanisms
please see main text
The functional EpoR that attenuates tissue damage is not nor-
mally, or only weakly, expressed in most tissues and is strongly
induced following injury (
36, 37
). EpoR expression level and the
number of receptors per cell is significantly lower than observed in
erythropoetic precursor cells and for that reason was reported as





































Search WWH ::

Custom Search