Biomedical Engineering Reference
In-Depth Information
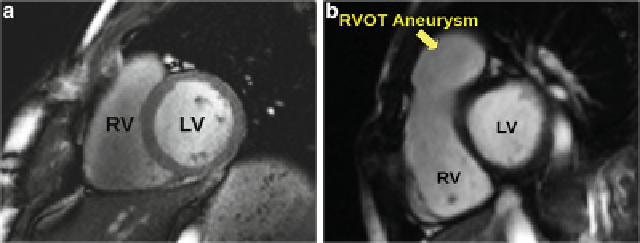
Fig. 5.1
Comparison between (
a
) a normal heart and (
b
) a Tetralogy of Fallot heart
which control one way blood flow from the right ventricle to the pulmonary artery
can be destroyed completely or damaged, causing blood to leak back to the right
ventricle. The long-term outcome of this condition is right ventricular re-modeling
caused by the regurgitated blood (Fig.
5.1
). Nowadays, patients undergo follow
up operations to reduce this post-operative sequelae. In particular, the valves are
replaced with an artificial device to reduce the regurgitation. A clinical challenge
for these patients is determining the optimal time for intervention. On the one hand,
it is preferable to wait as long as possible before performing such operations since
the artificial devices have a limited life-span resulting in the need for repeat follow-
up operations. Either open heart surgery or percutaneous valve replacement may
be required, depending on the diameter of the pulmonary annulus. These therapies
carry some danger, so minimizing the frequency and total number of surgeries is
crucial for these patients. On the other hand, the heart undergoes re-modeling due
to the regurgitated blood producing volume overload in the right ventricle and if
left long enough this damage can be irreversible. Determining the optimal time for
intervention is a trade-off between maximizing the time between operations and
minimizing damage to the heart.
Therefore, the clinical application for this condition is to better understand how
the heart evolves over a large period of time, often decades, with and without
surgery, with the main goal to be able to predict the optimal time for intervention.
However, due to the large variability of shape, the optimal time, placement and size
of the artificial device can be difficult to determine. Furthermore, the complexity
of the biological mechanisms involved in heart growth hinders the development of
a direct model of cardiac re-modeling. Statistical shape analysis can therefore be
employed to aid in further understanding the pathology to assist cardiologists with
diagnosis, therapy planning, and long term prognosis. More particularly, we are
interested in determining quantitative measures of the shape that correlate with the
cardiac function and the severity of the disease in these patients (bio-markers of the
disease). Such bio-markers could be used to determine the severity of the disease
when regurgitation cannot be assessed or to provide structural information that may
appear before deterioration of the blood dynamics.
Search WWH ::

Custom Search