Agriculture Reference
In-Depth Information
Lm
Cm
Mu
G
L
50
μ
m
Fig. 3.6
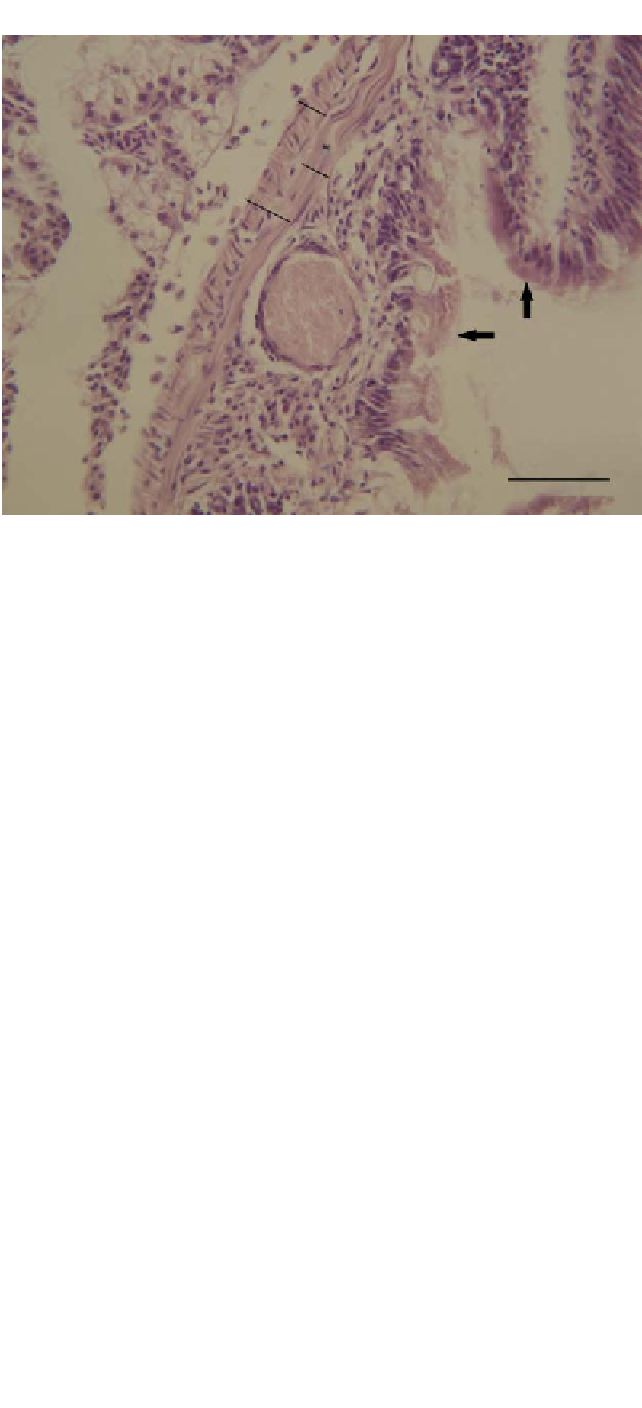
Light microscopy (H&E staining) transverse section of the intestine of zebrafish with clinical signs
of chronic mycobacteriosis. A lesion (granuloma, G) in the submucosa is indicated by the formation of
fibrous connective tissue around a small (
∼
50
μ
m) focus of acellular material. Key: arrow, epithelium; Cm,
circular muscle; L, lumen; Lm, longitudinal muscle; Mu, muscularis. Scale bar
=
50
μ
m. (Source: Kuehlwein
et al
., unpublished.) For colour detail see Plate 8.
Mycobacterium
spp. can survive and replicate within macrophages which allows them to
evade the host immune system. Mycobacteriosis causes ulcerations of the skin, emaciation,
and granulomatous lesions (organized collections of macrophages). Internally, grey-white
granulomas develop in the liver, kidney, spleen, heart, muscles and intestine (Figure 3.6).
There is presently no cure for mycobacteriosis. Mycobacterial infections of fish are zoonotic,
which means the organisms can cause disease in humans. Infected fish release the organism
from skin and gill lesions, and shed them from the GI tract. Infection can be spread when
fish have direct contact with infective material or ingest infected tissue. Examples of this
are from the early history of the salmon industry where fish were fed unpasteurized fish
waste which subsequently caused a serious problem with mycobacteriosis. There has been
a dramatic increase in the use of small fish in research, especially zebrafish
Danio rerio
.
One of the most common diseases of zebrafish is mycobacteriosis. Watral and Kent (2007)
conducted a study with intraperitoneal injection of various
Mycobacterium
spp. and recorded
mortalities and conducted histological appraisal.
Mycobacterium marinum
isolates caused
100% infection and between 30% and 100% mortality. None of the other
Mycobacterium
spp.
(
Mycobacterium peregrinum
and
Mycobacterium chelonae
) caused significant mortalities.
Harriff
et al.
(2007) established infection in zebrafish with both
M. peregrinum
and
M.
marinum
, using both bath and oral challenge, and concluded that the intestine was the primary
infection route (with high mycobacterium isolation from the intestine) and that
M. marinum
caused a higher number of clinical infections than
M. peregrinum
.


















Search WWH ::

Custom Search