Biology Reference
In-Depth Information
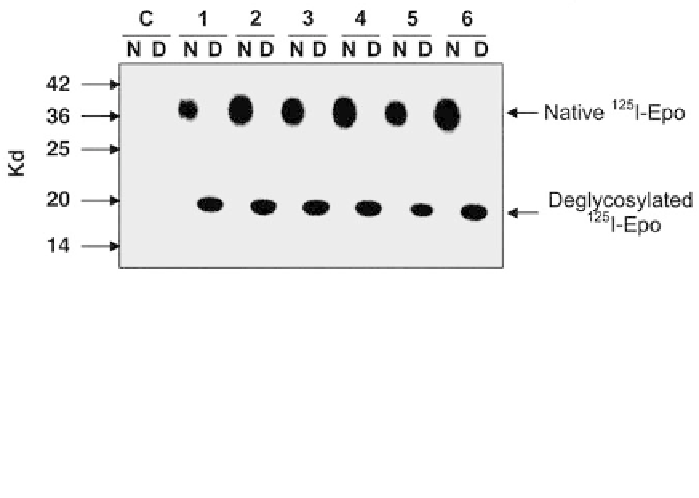
Figure 3. Anti-EPO neutralizing antibodies recognized the protein part of the EPO molecule.
125
I-EPO
was sequentially deglycosylated by incubating for one hour at 37 °C with
Arthrobacter ureafaciens
neuraminidase and for 18 hours with a mixture of O-glycosidase, endoglycosidase F and N-glycosi-
dase F (all glycohydrolases were from Roche, Mannheim, Germany). Native (N) and deglycosylated
(D)
125
I-EPO were then immunoprecipitated with serum from six patients with pure red cell aplasia
due to neutralizing anti-EPO antibodies or control serum (C). Immunoprecipitates were then analyzed
by polyacrylamide gel electrophoresis and autoradiography.
blood cell production, limited by their disease status. None was treated with
rHuEPO again. The number of studied cases is still too low to draw any reli-
able conclusions concerning the efficiency of the various immunosuppressive
therapies. Clearly, it is of the utmost importance not to challenge the antibody-
inducing rHuEPO by the use of another type of rHuEPO including darbepoet-
in alfa, since all antibodies that we have tested cross-reacted with all available
erythropoietic proteins. Theoretically, all erythropoietic proteins should be
able to boost antibody production in patients. An intriguing observation is that
anti-EPO antibodies disappeared in several patients and that these patients then
recovered red blood cell production, thus showing that these patients produced
endogenous EPO. The disappearance of antibodies seems to be hastened in
patients treated with immunosuppressive therapy, but antibodies also disap-
peared in some untreated patients. Thus, it appears that endogenous EPO pro-
duction is unable to boost antibody production. Whether this is due to the
properties of endogenous EPO or to the low amounts of endogenous molecules
produced in patients with chronic renal failure is unknown. We did not succeed
in measuring EPO concentration in serum samples containing anti-EPO anti-
bodies. Nevertheless, we also observed the spontaneous disappearance of anti-
EPO antibodies in the single patient who did not have chronic renal failure and
was not treated with rHuEPO. In contrast to patients with chronic renal failure,
patients without chronic renal failure should not have decreased production of
endogenous EPO. EPO production was probably strongly increased due to
anemia in this latter patient, suggesting that the spontaneous disappearance of
anti-EPO antibodies is probably not due to the low concentrations of endoge-
nous EPO produced in patients with chronic renal failure.