Biology Reference
In-Depth Information
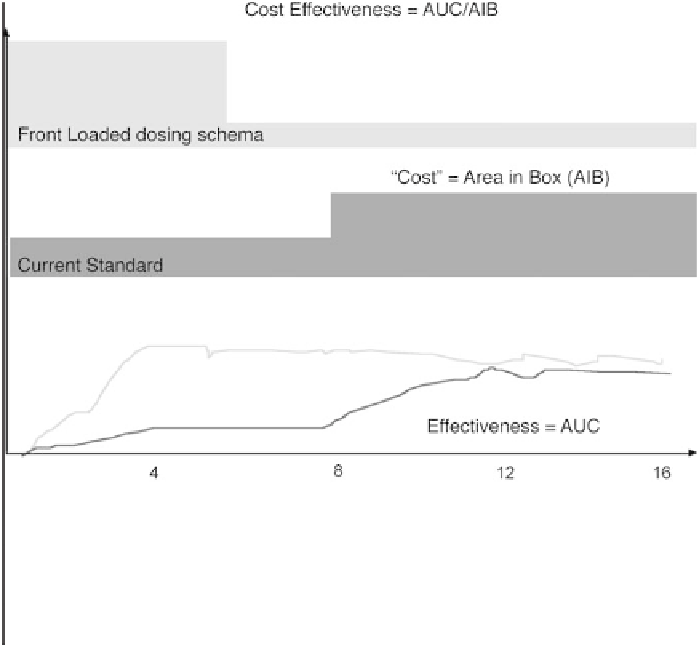
Figure 3. A theoretical schema for improving both patient benefit and cost effectiveness of erythro-
poietic therapy in oncology. For oncology patients, for whom rapid increases in hemoglobin are desir-
able, it may be more appropriate to begin therapy with optimal dosing and titrate down rather than to
adopt an approach of starting suboptimal and titrating up, an approach better suited to dialysis
patients.
thropoietic therapy, and a decrease in the doses of erythropoietic agents
required to maintain target hemoglobin concentrations [78-81]. Because can-
cer is a chronic inflammatory illness, with both decreased gastrointestinal
absorption of iron and an inflammatory blockade, compromising access by the
erythron to body iron stores, the potential of parenteral iron to decrease the
required doses of erythropoietic agents and to enhance hematologic response
must be seriously considered. In one randomized trial in anemic patients with
cancer who were not severely iron deficient, parenteral iron was associated
with enhanced response to epoetin alfa, compared with either oral iron or no
iron therapy; oral iron had no apparent effect [81]. Whatever the optimal
schedule and dose of erythropoietic agents that emerges from future clinical
trials, it appears likely that the addition of parenteral iron will enhance patient
benefit and/or lower the requisite dose of the erythropoietic agent.
New outcomes
An important issue in erythropoeitic therapy in oncology is the cost of
these agents, which is substantial and relatively simple to calculate. To ration-