Biology Reference
In-Depth Information
CoDx
CoDx
Initial Development
Initial Development
Prototype Assay
Prototype Assay
Investigational Assay
Investigational Assay
Commercial Assay
Commercial Assay
cobas
®
BRAF test
used to screen for
Phase II and Phase III
cobas
®
BRAF test
used to screen for
Phase II and Phase III
External 2-site validation
study complete
External 2-site validation
study complete
V600E assay
initiated
Plexxikon-RMS
CoDx agreement
V600E assay
initiated
Plexxikon-RMS
CoDx agreement
Prototype used to
screen for Phase I
Extension
Prototype used to
screen for Phase I
Extension
PMA
PMA
External 2-site
validation study
begins
External 2-site
validation study
begins
FDA approval &
CE-marking
FDA approval &
CE-marking
IDE approval for
prototype assay
IDE approval for
prototype assay
2005
2005
2006
2006
2007
2007
2008
2008
2009
2009
2010
2010
2011
2011
PLX 432 IND
PLX 432 IND
Phase I results
Phase I results
BRIM-2 results
BRIM-2 results
NDA & MAA
NDA & MAA
BRIM-3 results
BRIM-3 results
Roche-Plexxikon
Rx Agreement
Roche-Plexxikon
Rx Agreement
FDA approval
FDA approval
Rx
Rx
Preclinical
Preclinical
Phase I
Phase I
Phase II and III
Phases II and III
Commercial
Commercial
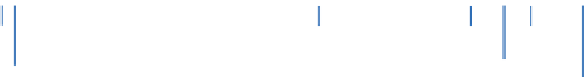
FIGURE 2.2
Milestones in the co-development of vemurafenib and the cobas® 4800 BRAF V600 Mutation Test.
(Reprinted from Lopez-Rios et al.
[72]
.)
showed a 53% response rate in a 132 patient Phase II study in individuals with melanoma
positive for the BRAF V600E mutation
[70]
and a > 50% overall response rate in a 675 patient
Phase III study comparing vemurafenib with dacarbazine in individuals with previously
untreated or unresectable stage IIIc or stage IV melanoma positive for the BRAF V600E muta-
tion
[71]
. All clinical data, including the results from the diagnostic assay, were submitted
to the FDA in May of 2011, with the concurrent approval of the diagnostic assay and vemu-
rafenib in August 2011. The overall time period of less than five years (see
Fig. 2.2
for timeline
of co-development of vemurafenib and the BRAF V600E diagnostic) between the filing of the
investigational new drug application and the FDA approval of vemurafenib highlights the key
value of identifying predictive biomarkers to select the right drug for the right patient.
2.2.2.3 Drug Metabolism
UGT1A AND IRINOTECAN
Irinotecan is a topoisomerase I inhibitor used to treat several solid tumor types, includ-
ing CRC, in combination with other chemotherapeutic agents. Inhibition of topoisomerase I
by irinotecan and its active metabolite, SN-38, prevents re-ligation of single-stranded DNA
breaks induced during cellular replication
[73,74]
. Uridine diphosphate glucuronosyltrans-
ferase 1A1 (UGT1A1) is a hepatic enzyme primarily responsible for conjugation of bilirubin
and endogenous hormones
[73,74]
. UGT1A1 also catalyzes the glucuronidation of SN-38,
the active metabolite of irinotecan and the main source of treatment-related toxicity
[73-75]
.
A recent meta-analysis demonstrated that genetic variation in UGT1A1 is moderately pre-
dictive of severe irinotecan-induced hematologic toxicity and neutropenia at intermediate
doses of irinotecan and strongly predictive at high doses (>250 mg
/
m
2
), but at low doses
these patients have a comparable incidence of toxicity compared to other patients
[73-76]
.
Therefore, knowledge of a patient's UGT1A1 polymorphism status could guide the selec-
tion of appropriate starting dosages, reducing the risk of severe toxicity and improving the
chances that therapy can be maintained. The most studied of the UGT1A1 polymorphisms
is UGT1A1*28, which results in reduced UGT1A1 activity, affecting the elimination of drug








Search WWH ::

Custom Search