Information Technology Reference
In-Depth Information
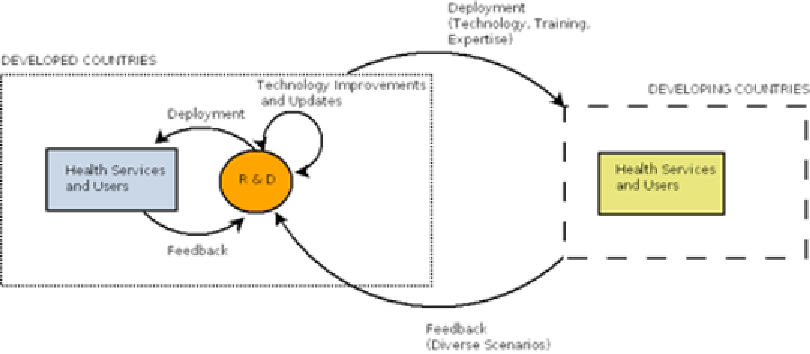
Figure 3. Research/development/deployment relationship between developed and developing countries
Treatment and Tracking
of Outpatients
there is a lack of proper regulatory frameworks
for centralized health database design. There is
also a scarcity of technical expertise and proper
education and sophistication for such databases.
Many private agencies and firms, usually in the
developed world, contribute immensely to the data
gathering for such databases. A good example of
one such firm is HDS (Healthcare Data Solutions),
which allows access to a full database (privately
maintained) using smartphone applications to over
100,000 medical prescribers, providing informa-
tion about doctor's offices, names, hospitals, and
pharmacies in the United States. There are many
other firms that also collect statistical information
about diseases.
As another example, the World Health Orga-
nization (WHO) currently maintains the Global
Health Observatory (http://www.who.int/gho/
en/, 2010), which is open to governments and
organizations. It is an interface that provides ac-
cess to various health data and analyses. It also
provides access to a full health database, which
lists (among other statistics): mortality, the burden
of disease, infectious diseases, risk factors, and
health expenditures. This work is commendable,
but with respect to the developing world, proper
education on interpreting this data and how to
effectively use it to analyze local health needs
and health preparedness are needed.
It is very important to track and assess the symp-
toms and treatment regimes for patients living
with life threatening diseases such as HIV/AIDS.
Such tracking can lead to an improvement in the
quality of life and can also lead to early detec-
tion of potential relapses in patient health. Such
palliative care is hard to come by in developing
countries. Most developing countries provide
care to such patients in outpatient settings, with
almost no steps being taken to provide palliative
care to the suffering population. Countries such
as Vietnam have tried to integrate palliative care
into existing treatment services (Kimberly Green
et al., 2010), but the vision for a proper policy on
how to achieve this is often muddled. There is
no clear guidance on how to operationalize this
sort of integration. A recent survey tested the
success of palliative care intervention in clinics,
which included tools to assess and treat pain and
other symptoms, mental health and social support
screening, counseling services, etc. The survey
received positive responses in favor of the success
of this intervention in clinics. There are techno-
logical hurdles to achieve this care remotely for
outpatients without them having to visit a clinic
physically and to monitor their own statistics.
Search WWH ::

Custom Search