what-when-how
In Depth Tutorials and Information
in association with injury. To help probe into the mecha-
nistic aspects of how the mutant BRIL causes such appar-
ently different consequences on bone, more suitable
animal models will have to be generated.
CLINICAL AND RADIOLOGIC
MANIFESTATIONS
Features Common to OI
OI type V patients do not have blue sclera and show
moderate bone fragility and moderate deforming ten-
dency of the spine and extremities. Lumbar spine BMD
z-scores (before bisphosphonate treatment) ranged
from −7.7 to −0.7, with a median of −5.3 in a series of 42
patients.
13
Most patients are short, but some are above
average. Age- and gender-matched z-scores for height
ranged from −8.7 to 1.88.
11,13,27
Scoliosis develops in more
than half of the patients.
11,27
Hearing loss is rare but can
affect some patients.
11
Wormian bone is not uncommon in
OI type V. An incidence of more than 10 Wormian bones
visible on a skull radiograph was reported as 35% in OI
type I, 73% in type V, 78% in type IV, and 96% in type III,
showing a correlation with the severity of the disease.
28
In
other series of OI type V, the incidence of Wormian bone
was reported as high as 94%.
29
Patients with OI type V
do not show generalized ligamentous laxity.
8
Soft tis-
sues such as skin, fasciae, tendon and ligament seem to
have normal texture in contrast to thin and friable tissues
in other types of OI. It is noteworthy that the severity of
the clinical manifestation is markedly variable patient-
to-patient even within a family, which includes bone fra-
gility, height, ambulatory status and disability from pain
and joint stiffness.
13
There are reports of fatality in early
childhood from pulmonary complications
13
and of wheel-
chair-bound cases.
11,13
However, some patients are living
very normal lives except for limited forearm rotation, e.g.,
one patient in our series in his thirties successfully served
in the army and is currently playing on an amateur soccer
team.
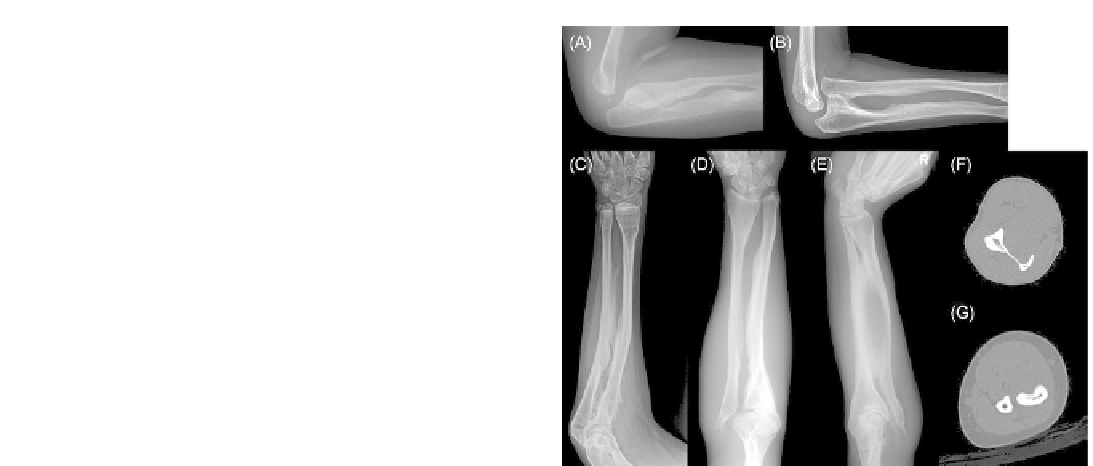
FIGURE 20.5
Radiographic findings of the forearm and elbow.
(A) Bulbous proximal ends of the radius and ulna along with bony
excrescences at the interosseous side in an 8-month-old girl. (B) A
7-year-old boy showed radial head dislocation and bony excrescences
at the interosseous borders of the radius and ulna. (C) A 14-year-old
boy showed radioulnar interosseous membrane ossification, but no
radial head dislocation. (D) A 30-year-old man showed radial head
dislocation and bony excrescence on the radial and ulnar diaphysis.
(E, F). A 50-year-old man showed advanced radioulnar interosseous
membrane ossification connecting the two bones and radial head dis-
location. The CT image shows ossification of the interosseous mem-
brane. (G) Bony excrescence along the interosseous border rather than
ossification of the interosseous membrane is noted on the forearm CT
image of a 9-year-old girl.
radius and ulna by a bony bridge (
Figure 20.5E and F
).
The range of forearm rotation - supination and prona-
tion - is limited to varying degrees. Even with significant
RUIMO, many patients maintain the functional use of
their forearm in daily living activities. Considering the
bony excrescence appearance in some patients, RUIMO
may be a site-specific form of subperiosteal bone forma-
tion, sharing the same pathogenic mechanism of para-
doxical dysregulated osteogenesis as in HC, heterotopic
ossification and MRB.
Radioulnar Interosseous Membrane Ossiication
(RUIMO) and Limitation in Forearm Rotation
RUIMO is the hallmark of OI type V, present in all
the patients except for one among the reported series to
varying degrees,
1,27,29,30
and is the most pathognomonic
sign (
Figure 20.5
). It is always observed on the ulna, and
frequently on the radius. In some patients, it looks like an
ossified interosseous membrane (
Figure 20.5C, E and F
),
but in others, it looks more like a bony excrescence at the
interosseous margin of the radius/ulna diaphysis
4,8,29,31
(
Figure 20.5A, B, D and G
). It seems to progress with age.
Some adult patients show complete connection of the
Radial Head Dislocation (RHD)
RHD is one of the conspicuous clinical and radio-
graphic signs of OI type V (
Figure 20.5E and F
). It is not
specific to OI type V, but is most common among the
subtypes of OI. Fassier et al. analyzed 489 upper limbs of
254 OI patients, reporting a significantly high frequency
of radial head malalignment in OI type V (86%) while
those in the other types ranged from 0 to 29%.
32
RHD
along with calcification of the interosseous membrane is
the most pathognomonic sign of OI type V. RHD in OI
type V was observed as early as 2 months of age
29
and
hence should be included in the differential diagnosis of